Is Your Sleep Disorder Linked to a Vitamin Deficiency?
According to health experts, vitamin D1,2 and sleep3,4 deficiencies are at epidemic proportions. It also appears they are related, as vitamin D levels affect your sleep quantity and quality.5 Sleep is an essential strategy for optimal health and immune support, and is at the heart of your circadian rhythm.
You may have heard your circadian rhythm referred to as your body clock. It's a natural, biological timer present in your cells that helps the body recognize sleepiness and wakefulness throughout a 24-hour period. Sleep is vital to remaining alert and awake during the day. But did you know that if you don't get enough sleep, nerve connections begin to break down in your brain?
Animal research6 published in the Journal of Neuroscience looked at the astrocyte activity in the brain of four groups of mice. Astrocytes are a type of brain cell that normally gets rid of unnecessary nerve connections. In mice that were well rested, they noted 5.7% of brain synapses had activity indicating a breakdown of healthy nerve synapses.
In the mice that were sleep-deprived or chronically sleep-deprived the activity jumped to 8.4% and 13.5% respectively, demonstrating that chronic sleep deprivation raises the risk that astrocyte cells will break down healthy nerve synapses.
According to a Gallup poll7 in 2013, 40% of those asked got less than seven hours of sleep each night. Yet, in 1942, participants in the survey slept an average of 7.9 hours. This dropped to 6.7 hours in 1990 and remained nearly steady at 6.8 hours to 2013.
Data from the CDC8 show there appears to be a geographical component to sleep duration. They categorized short sleep duration by state, finding many of the people who slept less than seven hours resided in states east of a line through Michigan, Indiana, Kentucky and Alabama. In some cases, sleep deprivation is a choice, but in others sleep disorders impact quantity and quality, resulting in chronic deprivation.
According to the American Sleep Association,9 up to 70 million U.S. adults have some type of sleep disorder, including snoring, insomnia, obstructive sleep apnea, narcolepsy and disrupted sleep.
When asked, 37.9% of people reported unintentionally falling asleep at least one time during the day in the past 30 days. While vitamin deficiencies may not influence what time you choose to go to bed, they can influence your sleep quality once you get there.
Improve Sleep by Optimizing Vitamin D Levels
Vitamin D plays a significant role in optimizing health. Scientists are still discovering the many ways in which your body uses vitamin D for regulation and modulation. Although it is found in few foods, it is also a hormone your body makes through sensible exposure to sunlight.10
Fatty fish, such as wild-caught Alaskan salmon, is among the best food sources of vitamin D.11 Depending on how the animals are raised, beef liver, egg yolks and cheese may have small amounts of vitamin D, and mushrooms will provide varying amounts.
The combination of low vitamin D content in foods and spending many hours indoors12,13 each day has likely contributed to the number of people who are deficient in vitamin D. Your serum level of 25-hydroxy vitamin D (25(OH)D) is the indicator used to measure the vitamin in your body.14
Research on Vitamin D and Sleep
Several studies have found a link between lack of sleep, sleep disorders and vitamin D deficiency. In 2012, Dr. Stasha Gominak, featured in the interview below, published a study15 in which she and her colleague used a two-year uncontrolled trial to evaluate the effect vitamin D supplementation had on neurological complaints and abnormal sleep patterns.
They engaged 1,500 people, in whom they maintained a narrow range of 25(OH)D levels between 60 nanograms per milliliter (ng/mL) and 80 ng/mL. These patients showed improvement in their sleep patterns and neurological symptoms.16
Later studies by other teams of researchers found similar results. One paper17 published in 2014 suggested that recent reports of vitamin D deficiency may increase symptoms of airway muscle myopathy, chronic rhinitis and/or adenotonsillar hypertrophy, which may lead to obstructive sleep apnea.
One study in 2015 showed low levels of serum 25(OH)D in older men decrease sleep duration and efficiency,18 and a systematic review published in 2018 found vitamin D deficiency was linked to a higher risk of sleep disorders.19
Also in 2018,20 a team of researchers evaluated vitamin D receptor genetic polymorphic variations and the impact serum concentration had on the susceptibility for obstructive sleep apnea syndrome. They found that one polymorphism explained 14.5% of the variability in serum concentration and was associated with excessive daytime sleepiness.
Finally, in late 2020, a paper21 published in Current Pharmaceutical Design sought to explore the role vitamin D plays in sleep regulation and the impact deficiency may have on sleep disorders. In a review of clinical trials and correlation studies they found vitamin D receptors and enzymes control activation expressed in the brain areas involved in sleep regulation. The team wrote:22
“Furthermore, vitamin D can affect sleep indirectly through non-specific pain disorders, correlated with alterations in sleep quality, such as restless legs syndrome and obstructive sleep apnea syndrome.”
A Healthy Gut Microbiome Supports Health and Sleep
In this fascinating interview with neurologist Dr. Stasha Gominak23 we discuss the relationship between your vitamin D status, microbiome health and sleep. During the interview, Gominak unpacks a large amount of information clearly and succinctly, describing how vitamin D modulates sleep and metabolism.
Many of her patients use fitness trackers that track sleep information, measuring slow-wave deep sleep, which is one of the sleep phases during which your body is paralyzed. She explains that the only time we are paralyzed is during restorative deep sleep, slow-wave sleep or REM sleep.24
As you consider fitness trackers, I would discourage the Fitbit for two primary reasons. First, it emits a green light that can interfere with sleep quality. Second, the company was recently bought by Google, which is siphoning your personal health and fitness data from these devices for their gain. Overall, I think the Oura ring is a superior device and it doesn't steal your personal data.
As you'll hear in the interview, Gominak used vitamin D and B12 to influence sleep patterns. Later, as patients' past symptoms were returning, she discovered that vitamin B5 may help improve sleep patterns and lower pain. However, in a few short months, she and dozens of her patients discovered that the supplementation levels were too high.
Once the supplementation was reduced, the symptoms went away. Gominak surmised that for some reason gut bacteria was not making enough vitamin B, which resulted in deficiency.25 Through a literature search, she found that B vitamins contribute to the production of acetylcholine in the brain and that vitamin D is one of three components that come together to make acetylcholine.
Optimizing Acetylcholine May Improve Nighttime Brain Repair
Acetylcholine is a neurotransmitter that has several important functions. Your parasympathetic nervous system depends on acetylcholine. Gominak shared that many papers have shown people with sleep disorders have excessive sympathetic tone. This in turn results in elevated epinephrine and norepinephrine, which are indicative of stress.
According to Gominak, an elevated sympathetic tone may be the result of an acetylcholine deficiency. Additionally, acetylcholine is necessary to help maintain alertness during the day and help you fall asleep at night. It's part of what allows your body to be paralyzed during deep sleep.
She believes once your vitamin D and B levels normalize, your brain can start repairing damage that had occurred during years of poor sleep.26 As a result, patients often find themselves sleeping longer than eight hours and remaining in REM sleep longer.
It's during this phase that cellular repair and regeneration is done. Without deep sleep, your body does not perform the needed cellular repair to maintain health, which is one reason why sleep dysfunction has such wide-ranging health effects. Another interesting piece of the puzzle that Gominak discovered is that sleeping longer increases the need for more B vitamins.
To optimize your gut microbiome to produce the needed B vitamins, she recommends having a vitamin D level above 40 ng/mL and using a B50 or B100 supplement for three months.27 This helps the microbiome produce the ideal amount of B vitamins on its own. She uses these strategies to improve sleep function and repair in her patients.
One-Two Punch for Sleep and Health: Melatonin and Vitamin D
You likely know that your circadian rhythm is in part dictated by the hormone melatonin. But did you know that vitamin D is involved in the pathways that produce melatonin in the pineal gland?28,29
Vitamin D has multiple effects on the body and as discussed, evidence demonstrates that low levels are associated with sleep disorders. An evaluation of clinical trials and correlation studies have shown that “Vitamin D has both a direct and indirect role in the regulation of sleep.”30
Melatonin, the hormone secreted by your pineal gland located near the center of the brain, is crucial for the regulation of your sleep cycle. With enough exposure to bright light during the daytime, the gland starts secreting melatonin during the evening darkness.31
As this amount increases the body prepares for sleep. When you stay up past dark using artificial light, especially light emitted by electronic devices, it inhibits melatonin production. Ideally, you would stop using electronics at least an hour or two before bedtime. This helps to raise your melatonin production and maintain a steady circadian rhythm.
Yet, like vitamin D, melatonin does more than support quality sleep.32 It’s also a potent antioxidant33 that plays an important role in cancer prevention.34 It’s thought to be important for brain, cardiovascular and gastrointestinal health,35 and has been shown to boost your immune function in a variety of ways.36
Melatonin was also found to be significantly reduced in adolescents diagnosed with Type 1 diabetes.37 In one paper,38 researchers suggested melatonin may improve the treatment of bacterial disease and combat sepsis. In 2020, sepsis and tissue oxygenation expert Dr. Paul Marik and colleagues proposed melatonin as an adjunctive treatment in severe sepsis and septic shock.39
Optimize Your Vitamin D Level
You know that optimizing sleep is one important way to take control of your health. And as Gominak notes in this interview, your sleep quality and quantity are related to maintaining optimal levels of nutrients and vitamins.
For optimal health, immune function and disease prevention, you want a vitamin D blood level between 60 ng/mL and 80 ng/mL year-round. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L.
If you live in a sunny locale like Florida and practice sensible sun exposure year-round, you might not need any supplements. The DMinder app40 is a helpful tool to see how much vitamin D your body can make depending on your location and other individual factors.
Many, unfortunately, don’t get enough sun exposure for one reason or another, and in these cases, an oral vitamin D supplement may be required. Just remember that the most important factor here is your blood level, not the dose, so before you start, get tested so you know your baseline.
Here’s a summary of how to determine whether you might need an oral supplement, and your ideal dosage:
1. First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in GrassrootsHealth's personalized nutrition project, which includes a vitamin D testing kit. Once you know what your blood level is, you can assess the dose needed to maintain or improve your level.
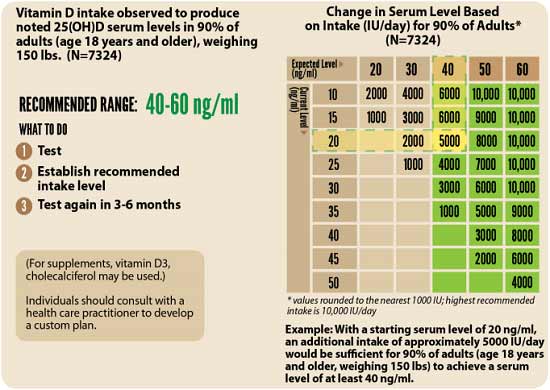
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. (To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5.) To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.41
Factors that can influence your vitamin D absorption include your magnesium42 and vitamin K243 intake. Magnesium is required for the conversion of vitamin D into its active form.44,45,46,47 If your magnesium level is insufficient, the vitamin D you ingest orally may simply get stored in its inactive form.48,49
Research by GrassrootsHealth50 shows you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
Your best bet is to take your vitamin D with both magnesium and K2. According to GrassrootsHealth,51 “combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually,” and “those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither.”
Data52 from nearly 3,000 individuals revealed 244% more oral vitamin D was required to get 50% of the population to achieve a vitamin D level of 40 ng/ml (100 nmol/L) if they weren’t concurrently also taking magnesium and vitamin K2.
3. Retest in three to six months — Remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
from Articles https://ift.tt/3EEfSQ6
via IFTTT