COVID-19 Pandemic Has Decimated Mental Health
America has had an epidemic of poor health long before SARS-CoV-2 appeared earlier this year. This is largely a result of industry propaganda influencing their choices of large amounts of processed foods that are high in carbs and industrially processed vegetable oils.
However, over the past several months, several polls discovered more about the impact of the COVID-19 pandemic response on mental health, and it’s not good. In the featured video, Glenn Greenwald, host of System Update, discusses the “crumbling of the U.S. social fabric” and explores the rise in “deaths of despair” from drugs and suicide brought on by the pandemic.
Anxiety, Depression and Suicide Are at All-Time Highs
Indeed, statistics show rates of depression, anxiety and suicide are currently at an all-time high.1,2 The Kaiser Family Foundation has conducted polls at regular intervals since the beginning of the pandemic. Here’s a quick summary of findings over time:
• In the early-April poll,3 45% of respondents said the pandemic had disrupted their lives “a lot,” with women (49%) being more disproportionally affected than men (40%). At the time, 52% worried they would lose their job, and 85% worried local businesses would have to permanently close due to loss of revenue.
• The late-July poll4 found that 60% of American adults still felt that the worst effects of the pandemic were still to come (down from 74% in early April5), and 53% now said that “worry and stress related to coronavirus has had a negative impact on their mental health.” Of respondents, 4 in 10 reported having trouble affording basic necessities or falling behind on bills.
• Poll results6 published in late August revealed economic hardships have negatively affected many people’s mental health “and created new barriers for people already suffering from mental illness and substance use disorders.”
As in the previous month, 53% of American adults said their mental health “has been negatively impacted due to worry and stress over the coronavirus;” 36% report having trouble sleeping, 32% have trouble eating, 12% report increased alcohol consumption and/or substance use and 12% report worsening of chronic health conditions due to worry and stress.
Those faring the worst are people sheltering in place, 47% of whom report negative health effects, compared to 37% of those not sheltering in place. Women with children under the age of 18 also report higher rates of mental health problems than male counterparts. Kaiser Family Foundation reports:
“More than 1 in 3 adults in the U.S. have reported symptoms of anxiety or depressive disorder during the pandemic (weekly average for May: 34.5%; weekly average for June: 36.5%; weekly average for July: 40.1%).” For comparison, from January to June 2019, the rate of anxiety or depressive disorder was 11%.
Stress Is Taking a Toll, CDC Finds
Similarly, a study7 by the U.S. Centers for Disease Control and Prevention published August 14, 2020, found 40.9% of the 5,412 respondents reported struggling with anxiety, depression or symptoms of trauma- and stressor-related disorder (TSRD) relating to the pandemic; 13.3% of American adults reported new or increased substance use as a way to manage stress, and 10.7% of adults said they’d seriously contemplated suicide in the past 30 days.
Unpaid caregivers for adults had the highest rate of suicidal ideation at 30.7%, followed by young adults, age 18 to 24 (25.5%) and essential workers (21.7%). Symptoms of trauma- and stressor-related disorder caused by the pandemic, increased substance use and suicidal ideation were all also more prevalent among employed than unemployed respondents.
Now, as noted by Greenwald in the video above, depression and suicide rates were seeing significant increases even before the pandemic, especially among younger people. This, despite the explosion of social media, where you can stay connected to people across vast distances 24/7.
This paradoxical result has been taken as evidence that social media simply cannot replace actual face-to-face interactions. We need physical contact. We need to be able to interact face-to-face.
Between lockdowns and mandatory mask orders, not only has physical contact been extinguished, but we also cannot see each other’s facial expressions when wearing masks. Both significantly contribute to the feeling of alienation and loneliness.
Antidepressant Use Has Skyrocketed
According to an April 16, 2020, report8,9,10 by Express Scripts, an employer-based pharmacy benefit management company, prescriptions for antidepressants have also skyrocketed, rising 34.1% between mid-February and mid-March, by which time stay at home orders had been issued for many parts of the U.S.
Combined, drugs for anxiety, depression and insomnia rose by 21%. Mirroring poll results, far more women have turned to antidepressants than men, with women increasing use by 40% compared to men, who had a 22.7% rise in prescriptions.11
June 3, 2020, The Food and Drug Administration reported12 that the antidepressant Zoloft had been added to the FDA’s list of drugs experiencing shortages due to increased demand. Increased antidepressant use has also been reported in Queensland, Australia.13
All of this is regrettable, considering studies14,15,16,17,18,19 have repeatedly shown antidepressants work no better than placebo for mild to moderate depression and come with a long list of adverse health effects.
According to a 2017 systematic review20 that included meta-analysis and trial sequential analysis of 131 placebo-controlled studies, all trials were at high risk of bias, thereby rendering their clinical significance “questionable.” None of the trials, even when reporting a positive result, met the threshold for clinical significance of three points on the depression score.
The authors also pointed out that “SSRIs significantly increase the risk of both serious and non-serious adverse events,” and that “The potential small beneficial effects seem to be outweighed by harmful effects.”
Suicide Rates Are Spiking
As one would expect, we are also seeing a rise in suicides. In a July 2020 Buck Institute webinar reported by Townhall,21 CDC director Robert Redfield stated that lockdowns and lack of school attendance have had a disproportionally negative impact on children and teens’ mental health. Among high school students — who are at very low risk of dying from COVID-19 — suicides and drug overdoses have surpassed the death rate for COVID-19.
“This is why I keep coming back for the overall social being of individuals,” Redfield said. “Let’s all work together and find out how we can find common ground to get these schools open in a way that people are comfortable and they’re safe."
Townhall pointed out that it’s unclear where Redfield got his data,22 but highlighted a May 21, 2020, report23 by ABC7 News, in which Dr. Mike deBoisblanc, at John Muir Medical Center in Walnut Creek, California, stated the hospital had “seen a year’s worth of suicide attempts” in just four weeks.
Trauma nurse Kacey Hansen was also quoted, saying, “What I have seen recently, I have never seen before. I have never seen so much intentional injury.” In March, FirstLink, a company that answers 211 helplines and the National Suicide Prevention Lifeline for North Dakota and parts of Minnesota, reported a 300% increase in call volume.24 Text conversations with the national Crisis Text Line were also double that of the normal volume during the week of March 15.25
The week of April 20, which, looking back, coincided with the peak of COVID-19 deaths in the U.S., suicides exceeded COVID-19 deaths in Tennessee,26,27 and in Knox County (one of the few areas in Tennessee where nonessential businesses were ordered to close), eight suicides took place within a span of just 48 hours during the third week of March.28
Meanwhile, only six patients died from COVID-19 in the entire state that week. In a statement, Knoxville, Tennessee, Mayor Glenn Jacobs said:29
“That number is completely shocking and makes me wonder if what we are doing now is really the best approach. We have to determine how we can respond to COVID-19 in a way that keeps our economy intact, keeps people employed and empowers them with a feeling of hope and optimism — not desperation and despair.”
Isolation Worsens Already Existing Mental Health Issues
A report released in April by The Well Being Trust predicts30 “deaths of despair” due to the COVID-19 pandemic may reach as high as 75,000. Psycom, which reported the results, noted:31
“The research has been clear on this one for years: isolation and loneliness is bad for our health — both physical and mental. According to a meta-analysis co-authored by Julianne Holt-Lunstad, PhD, a professor of psychology and neuroscience at Brigham Young University, lack of social connection heightens health risks as much as smoking three-quarters of a pack of cigarettes a day, every day.
‘There is robust evidence that social isolation and loneliness significantly increase risk for premature mortality, and the magnitude of the risk exceeds that of many leading health indicators,’ Holt Lunstad says. The coronavirus has obviously exacerbated the problem.”
In a related article, Psycom notes that:32
“The effects of this crisis are more far-reaching than heightened anxiety, which pretty much everyone is feeling. There are also trickle-down effects to those with addiction and behavioral disorders like OCD, ADHD, and substance abuse.
Along with the good that social distancing can do for our own health and society in general, it also increases feelings of isolation, loneliness, stress, and fear — all of which can be triggers that make many mental illnesses infinitely worse.”
The article goes on to address what people struggling with nine of the most common mental health problems can do to cope better. This includes those with anxiety, depression, obsessive-compulsive disorder, substance abuse and eating disorders, ADHD, bipolar disorder, schizophrenia and post-traumatic stress disorder. For more details about each of those, please refer to the original Psycom article.33
Intentional and Unintentional Deaths Reported by CDC
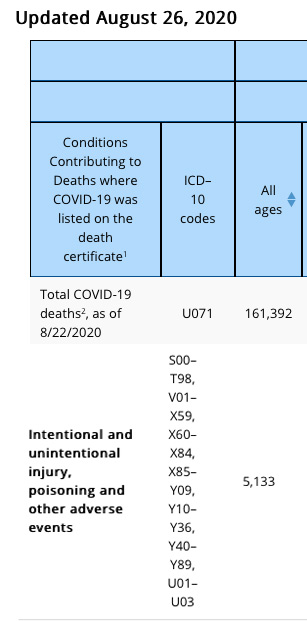
According to data34 released by the CDC August 26, 2020, only 6% of the total COVID-19-related death toll had COVID-19 listed as the sole cause of death on the death certificate. Six percent of 161,392 is 9,683. “For deaths with conditions or causes in addition to COVID-19, on average, there were 2.6 additional conditions or causes per death,” the CDC states.
Now, we’ve heard reports of accident victims being listed as COVID-19 deaths, and Table 3 in this August 26 report is granular enough that we can see that a total of 5,133 “COVID-19-related deaths” also had “intentional or unintentional injury, poisoning or other adverse events” listed on the death certificate.
This number likely also contains suicides where the individual was found to test positive for SARS-CoV-2, or was suspected of testing positive. (Please note, these data are accurate as of this writing, as shown in the partial screenshots below. The CDC does not notate when data are altered as new death certificates come in, so the numbers may therefore be different from what is reported here, depending on when you’re looking at it. For the most up-to-date figures, see the CDC’s website.35)
The Difference Between Being Scared and Being Fearful
Fear is the primary emotion that the technocrats are using to manipulate and coerce their tyrannical controls. It is the most powerful tool at their disposal and highly effective which is why it is being deployed.
As explained in “You Can Control Fear,” there’s a difference between being scared and being fearful. Right now, the whole world is holding its proverbial breath in anticipation for what might come next. It’s easy to feel fearful, considering the daily barrage of bad news.
However, understanding the difference between being scared and living in fear can be very helpful, as fear has a paralyzing effect while being scared primarily heightens alertness. Novel threats raise a person's level of anxiety to a greater degree than familiar threats, even when they have the same or similar consequences. This is thought to be related to activity in your amygdala, which processes emotions.36
Ryan Holiday, media strategist and author of 10 books, including “The Daily Stoic” and “The Obstacle Is the Way,” writes:37
“Being afraid? That’s not fight or flight. That’s paralysis. That only makes things worse. Especially right now. Especially in a world that requires solutions to the many problems we face. They’re certainly not going to solve themselves. And inaction (or the wrong action) may make them worse, it might put you in even more danger. An inability to learn, adapt, to embrace change will too.”
While fleeting feelings of concern are expected when faced with new experiences, when such feelings are allowed to continuously dominate, paralysis can set in. To thrive in times of great uncertainty and fear, Holiday stresses the importance of training, education and preparation, which are the foundations of courage.38
The difference between being fearful and being scared is that fear paralyzes your ability to evaluate what's happening and to make decisions. But preparation and information help you to make decisions and act, even when you're scared. This is the definition of courage — taking action despite being scared.
How to Reduce Fear and Find Courage
There are several strategies you can use to reduce fear and find courage. It is important to begin with the understanding that your thoughts engender feelings. Your emotions do not have a life of their own, but rather are dependent on your thinking.
So, one of the strategies you can use to reduce fear is to change the way you think about things. Yes, we’re dealing with many unknowns right now, but focusing on planning and preparation rather than getting locked into panic mode can go a long way toward safeguarding your mental health. Take the safety precautions you can take, and limit your exposure to the news.
Psychology Today39 recommends reducing anxiety by consuming positive news stories while keeping up with what’s going in the world. Also do your best to apply some critical thinking when reading the news.
It’s important to pay careful attention to “vague or loaded terms, cited statistics, and unstated assumptions.” In other words, don’t accept at face value what’s in the news but, rather, consider the information and ask questions about what you’re being told. Other stress- and depression-reducing techniques include:40
- Getting enough exercise
- Eating whole foods
- Limiting sugar
- Getting quality sleep
- Practicing meditation and mindfulness training
When you’re tired and your body doesn’t have adequate nutrition to function, you’re more apt to fall into the trap of fear-based thinking. Additional nondrug treatment strategies for depression can be found in “What Does the Best Evidence Say About Antidepressants?”
The Emotional Freedom Techniques
A strategy that can provide more immediate results is the use of Emotional Freedom Techniques, or EFT. In the video above, Julie Schiffman demonstrates a tapping strategy to relieve anxiety and other challenging emotions brought on by news and uncertainty about this pandemic and/or self-quarantining. If you aren’t familiar with EFT you’ll find a library of demonstrations at “Basic Steps to Your Emotional Freedom.”
The NET FAST Technique
Another alternative is the Neuro-Emotional Technique’s First Aid Stress Tool, or NET FAST, demonstrated in the video above. Firstaidstresstool.com also provides an excellent printable summary with visuals of the technique,41 which even a young child can do. Here is a summary of the FAST procedure:
- While thinking about an issue that is bothering you, place your right wrist, palm up, into your left hand. Place three fingers of your left hand onto the area of your right wrist where you can feel your pulse
- Place your open right hand on your forehead. Gently breathe in and out several times while concentrating on feeling the issue that bothers you
- Switch hands and repeat Steps 1 and 2
Suicide Prevention Resources
If you feel depressed, anxious or creeping despair, please do not hesitate to reach out to family, friends or any of the available suicide prevention services:
- The National Suicide Prevention Lifeline (U.S.) — Call 1-800-273-TALK (8255)
- Crisis Text Line — Text HOME to 741741 to connect with a crisis counselor
- Lifeline Crisis Chat — Chat online with a specialist who can provide emotional support, crisis intervention and suicide prevention services at suicidepreventionlifeline.org
- Alternatively, call 911, or simply go to your nearest Hospital Emergency Department
from Articles https://ift.tt/2FlNHfM
via IFTTT