Health, Fitness,Dite plan, health tips,athletic club,crunch fitness,fitness studio,lose weight,fitness world,mens health,aerobic,personal trainer,lifetime fitness,nutrition,workout,fitness first,weight loss,how to lose weight,exercise,24 hour fitness,
Labels
Technology
New Post
The role diets have on your hormones in every decade of your life
from Nutrition | body+soul https://ift.tt/2T6eX6B
Morning vs lunch vs evening: Sam Wood reveals when to exercise to lose weight
from Fitness | body+soul https://ift.tt/3caqmJW
5 things a naturopath does for optimal hormone health
from Health | body+soul https://ift.tt/32taaio
New compounds thwart multiple viruses, including coronavirus
from Top Health News -- ScienceDaily https://ift.tt/394sGA6
New CRISPR base-editing technology slows ALS progression in mice
from Top Health News -- ScienceDaily https://ift.tt/32AbU9J
Poor cleaning can jeopardize sterilization of medical tools
from Top Health News -- ScienceDaily https://ift.tt/2Pr2Ka2
Nanosize device 'uncloaks' cancer cells in mice and reveals them to the immune system
from Top Health News -- ScienceDaily https://ift.tt/2T2fqXg
Scientists discover new clue behind age-related diseases and food spoilage
from Top Health News -- ScienceDaily https://ift.tt/32s4FAw
New study allows brain and artificial neurons to link up over the web
from Top Health News -- ScienceDaily https://ift.tt/2HWmoqr
Dopamine fasting: Misunderstanding science spawns a maladaptive fad
The dopamine fast, created by California psychiatrist Dr. Cameron Sepah, has very little to do with either fasting or dopamine. As Sepah told the New York Times, “Dopamine is just a mechanism that explains how addictions can become reinforced, and makes for a catchy title. The title’s not to be taken literally.” Unfortunately, with such a snazzy name, who could resist? This is where the misconceptions begin.
What’s the thinking behind a dopamine fast?
What Sepah intended with his dopamine fast was a method, based on cognitive behavioral therapy, by which we can become less dominated by the unhealthy stimuli — the texts, the notifications, the beeps, the rings — that accompany living in a modern, technology-centric society. Instead of automatically responding to these reward-inducing cues, which provide us with an immediate but short-lived charge, we ought to allow our brains to take breaks and reset from this potentially addictive bombardment. The idea is that by allowing ourselves to feel lonely or bored, or to find pleasures in doing simpler and more natural activities, we will regain control over our lives and be better able to address compulsive behaviors that may be interfering with our happiness.
The six compulsive behaviors he cites as behaviors that may respond to a dopamine fast are: emotional eating, excessive internet usage and gaming, gambling and shopping, porn and masturbation, thrill and novelty seeking, and recreational drugs. But he emphasizes that dopamine fasting can be used to help control any behaviors that are causing you distress or negatively affecting your life.
You can’t “fast” from a naturally occurring brain chemical
Dopamine is one of the body’s neurotransmitters, and is involved in our body’s system for reward, motivation, learning, and pleasure. While dopamine does rise in response to rewards or pleasurable activities, it doesn’t actually decrease when you avoid overstimulating activities, so a dopamine “fast” doesn’t actually lower your dopamine levels.
Unfortunately, legions of people have misinterpreted the science, as well as the entire concept of a dopamine fast. People are viewing dopamine as if it was heroin or cocaine, and are fasting in the sense of giving themselves a “tolerance break” so that the pleasures of whatever they are depriving themselves of — food, sex, human contact — will be more intense or vivid when consumed again, believing that depleted dopamine stores will have replenished themselves. Sadly, it doesn’t work that way at all.
Fasting may simply be a technique to reduce stress and engage in mindfulness-based practices
Sepah recommends that we start a fast in a way that is minimally disruptive to our lifestyles. For example, we could practice dopamine fasting from one to four hours at the end of the day (depending on work and family demands), for one weekend day (spend it outside on a Saturday or Sunday), one weekend per quarter (go on a local trip), and one week per year (go on vacation).
This all sounds sensible, if not necessarily new or groundbreaking. In fact, it sounds a lot like many mindfulness practices and good sleep hygiene, in the suggestion of no screen time before bed.
However, people are adopting ever more extreme, ascetic, and unhealthy versions of this fasting, based on misconceptions about how dopamine works in our brains. They are not eating, exercising, listening to music, socializing, talking more than necessary, and not allowing themselves to be photographed if there’s a flash (not sure if this applies to selfies).
Misunderstanding science can create maladaptive behaviors
When you think that none of this is actually lowering dopamine, it’s kind of funny! Especially since avoiding interacting with people, looking at people, and communicating with people was never part of Sepah’s original idea. Human interaction (unless it is somehow compulsive and destructive) is in the category of healthy activities that are supposed to supplant the unhealthy ones, such as surfing social media for hours each day. In essence, the dopamine fasters are depriving themselves of healthy things, for no reason, based on faulty science and a misinterpretation of a catchy title.
Taking time out for mental rejuvenation is never a bad thing, but it’s nothing new
The original intent behind the dopamine fast was to provide a rationale and suggestions for disconnecting from days of technology-driven frenzy and substituting more simple activities to help us reconnect us with ourselves and others. This idea is noble, healthy, and worthwhile, but it’s certainly not a new concept. Most religions also suggest a rest day (for example, the Jewish Sabbath) or holidays without technological distractions, so that you can reflect and reconnect with family and community, Thousands of years of meditation also suggests that a mindful approach to living reaps many health benefits.
Unfortunately, the modern wellness industry has become so lucrative that people are creating snappy titles for age-old concepts. Perhaps that is how to best categorize this fad, if only we can get its proponents to look at us or speak to us, without disturbing their dopamine levels, in order to explain this to them.
The post Dopamine fasting: Misunderstanding science spawns a maladaptive fad appeared first on Harvard Health Blog.
from Harvard Health Blog https://ift.tt/2HTWVOu
Fur-friendly 'wearable for pets' and their humans
from Top Health News -- ScienceDaily https://ift.tt/2Psausz
Tone down your risk of skin cancer
from Top Health News -- ScienceDaily https://ift.tt/2wapGUA
Cellular metabolism regulates the fate decision between pathogenic and regulatory T cells
from Top Health News -- ScienceDaily https://ift.tt/2uB73bU
Women firefighters face high exposure to toxic PFAS chemicals
from Top Health News -- ScienceDaily https://ift.tt/2T2u0hi
Researchers make asthma breakthrough
from Top Health News -- ScienceDaily https://ift.tt/2w3y6Nt
Drinks with added sugars linked to lipid imbalance, which increases CVD risk
from Top Health News -- ScienceDaily https://ift.tt/2VuU8mZ
How your romantic attachment style affects your finances, well-being
from Top Health News -- ScienceDaily https://ift.tt/3aaYX93
Drinks with added sugars linked to lipid imbalance, which increases CVD risk
from Diet and Weight Loss News -- ScienceDaily https://ift.tt/2VuU8mZ
Pediatric Drug Poisoning Is on the Rise
Aside from causing a wide variety of side effects in those who take medications, the widespread routine use of pharmaceuticals also pose a serious risk to children who get their hands on them.
As of 2016, nearly half of the U.S. population were on at least one medication.1,2 Twenty-four percent used three or more drugs, and 12.6% were on more than five different medications.3 According to the 2016 National Ambulatory Medical Care Survey, 73.9% of all doctor’s visits also involved drug therapy.4
As one would expect, drug use dramatically increases with age. As of 2016, 18% of children under 12 were on prescription medication, compared to 85% of adults over the age of 60. While this trend is troubling enough, with prescription drugs now being a staple in most homes, the number of children suffering accidental poisoning is also on the rise.
Medications Pose Serious Risks to Young Children
According to a 2012 article5,6 in The Journal of Pediatrics that reviewed patient records from the National Poison Data System of the American Association of Poison Control Centers, 453,559 children aged 5 or younger were admitted to a health care facility following exposure to a potentially toxic dose of a pharmaceutical drug between 2001 and 2008.
In that time, drug poisonings rose 22%. Ninety-five percent of cases were due to self-exposure, meaning the children got into the medication and took it themselves, opposed to being given an excessive dose by error.
Forty-three percent of all children admitted to the hospital after accidentally ingesting medication ended up in the intensive care unit, and prescription (opposed to over-the-counter) medications were responsible for 71% of serious injuries, with opioids, sedative-hypnotics and cardiovascular drugs topping the list of drugs causing serious harm. As noted by the authors:7
“Prevention efforts have proved to be inadequate in the face of rising availability of prescription medications, particularly more dangerous medications.”
Keep All Drugs in Childproof Containers
If you’re older, you may recall your parents or grandparents would have a lockable medicine cabinet where drugs were stored. Few people keep their medications in locked cabinets or boxes these days, failing to realize the serious risk they pose to young children.
The hazard is further magnified if you sort your medications into easy-open daily pill organizers rather than keeping each drug in its original childproof container.
A 2020 paper8,9 in The Journal of Pediatrics, which sought to “identify types of containers from which young children accessed solid dose medications during unsupervised medication exposures” found 51.5% involved drugs accessed as a result of having been removed from its original childproof packaging.
Remarkably, in 49.3% of cases involving attention deficit hyperactivity disorder medications and 42.6% of cases involving an opioid, the drug was not in any container at all when accessed. In other words, the child found the pill or pills just laying out in the open. In 30.7% of all cases where a child ingested a drug, the exposure involved a grandparent’s medication. As noted by the authors:
“Efforts to reduce pediatric SDM [solid dose medication] exposures should also address exposures in which adults, rather than children, remove medications from child-resistant packaging.
Packaging/storage innovations designed to encourage adults to keep products within child-resistant packaging and specific educational messages could be targeted based on common exposure circumstances, medication classes, and medication intended recipients.”
Teen Drug Overdoses Are Also on the Rise
While infants are notorious for putting anything and everything in their mouth, making them particularly vulnerable to accidental drug exposures, drug overdoses, particularly those involving opioids and benzodiazepines, are also becoming more prevalent among teens with access to these drugs.
According to a 2019 study10 published in the journal Clinical Toxicology, 296,838 children under the age of 18 were exposed to benzodiazepines between January 2000 and December 2015. Over that time, benzodiazepine exposure in this age group increased by 54%. According to the authors:11
“The severity of medical outcomes also increased, as did the prevalence of co-ingestion of multiple drugs, especially in children ages 12 to <18 years. Nearly half of all reported exposures in 2015 were documented as intentional abuse, misuse, or attempted suicide, reflecting a change from prior years …
Medical providers and caretakers should be cognizant of this growing epidemic to avoid preventable harm to adolescents, young children, and infants.”
A similar trend has been found with opioids. A 2017 study12 looking at prescription opioid exposures among children and adolescents in the U.S. between 2000 and 2015 found:
“Poison control centers received reports of 188,468 prescription opioid exposures among children aged<20 years old from 2000 through 2015 … Hydrocodone accounted for the largest proportion of exposures (28.7%), and 47.1% of children exposed to buprenorphine were admitted to a health care facility (HCF).
The odds of being admitted to an HCF were higher for teenagers than for children aged 0 to 5 years or children aged 6 to 12 years. Teenagers also had greater odds of serious medical outcomes … The rate of prescription opioid-related suspected suicides among teenagers increased by 52.7% during the study period.”
Commonsense Precautions
The U.S. Centers for Disease Control and Prevention promotes and supports the Up and Away and Out of Sight campaign, which centers “around several simple, data-driven actions that parents and caregivers can take to prevent medication overdoses in the children they care about and care for.”13 These commonsense precautions include the following:14
- Store your medications (and supplements) in their original packaging in a place your child cannot reach. Don't store medications in your nightstand, purse or end table where little hands are likely to explore and find them. Any medication stored in the refrigerator should be in childproof packaging. Also make sure drugs are safely stored in areas your child visits frequently, such as a grandparent’s house or a baby sitter.
- Put all medications away after each use.
- Make sure to relock the safety cap after each use.
- Teach your children about medicine safety; never tell them medicine is “like candy” in order to get them to take it.
- Remind guests to place bags, purses and coats that have medicine in them in a safe place while visiting.
What to Do in Case of Accidental Drug Exposure
Be sure to keep the Poison Help number in your phone, and make sure your baby sitter or caregiver has it. In the U.S., the Poison Help number is 800-222-1222. If you suspect your child has taken a prescription or OTC medication, even if he or she is not yet exhibiting symptoms, call the Poison Help line immediately.
If you’re unsure what medication your child may have taken, call 911 or the emergency number in your area for transportation to the nearest medical facility. Although your child may appear fine in the initial minutes, this can rapidly change. You want to start treatment as soon as possible to reduce the risk of permanent damage or potential death.
Remember to bring with you the names of any medications your child may have accidentally ingested, as well as any medications your child has taken in the past 24 hours as prescribed by their doctor, any allergies they have, and any changes or symptoms you may have observed.
Unfortunately, symptoms of a medication overdose can vary widely, depending on the drug, dosage and age of the child. That said, symptoms of an overdose may include:15
|
Nausea |
Vomiting or diarrhea |
|
Drooling or dry mouth |
Convulsions |
|
Pupils that grow larger or shrink |
Sweating |
|
Loss of coordination and/or slurred speech |
Extreme fatigue |
|
Yellow skin or eyes |
Flu-like symptoms |
|
Unusual bleeding or bruising |
Abdominal pain |
|
Numbness |
Rapid heartbeat |
Should your child exhibit any of the following symptoms, call 911 (in the U.S.) immediately:16
|
Won’t wake up |
Can’t breathe |
|
Twitches or shakes uncontrollably |
Displays extremely strange behavior |
|
Has trouble swallowing |
Develops a rapidly spreading rash |
|
Swells up in the face, including around the lips and tongue |
Opioid Epidemic Takes Toll on Pediatric Population
It’s crucial to realize that many drugs can be life threatening to a young child, even in low doses. This is particularly true for opioids and buprenorphine, a drug used to treat opioid dependence. As noted in a 2005 paper17 on opioid exposure in toddlers:
“Ingestions of opioid analgesics by children may lead to significant toxicity as a result of depression of the respiratory and central nervous systems. A review of the medical literature was performed to determine whether low doses of opioids are dangerous in the pediatric population under 6 years old.
Methadone was found to be the most toxic of the opioids; doses as low as a single tablet can lead to death. All children who have ingested any amount of methadone need to be observed in an Emergency Department (ED) for at least 6 h and considered for hospital admission.
Most other opioids are better tolerated in ingestions as small as one or two tablets. Based on the limited data available for these opioids, we conclude that equianalgesic doses of 5 mg/kg of codeine or greater require 4 to 6 h of observation in the ED.
Data for propoxyphene and all extended-release preparations are limited; their prolonged half-lives would suggest the need for longer observation periods. All opioid ingestions leading to respiratory depression or significant central nervous system depression require admission to an intensive care unit.”
Similarly, a 2006 paper18 on the adverse effects of unintentional buprenorphine exposure in children noted that:
“Buprenorphine in sublingual formulation was recently introduced to the American market for treatment of opioid dependence. We report a series of 5 toddlers with respiratory and mental-status depression after unintentional buprenorphine exposure.
Despite buprenorphine's partial agonist activity and ceiling effect on respiratory depression, all children required hospital admission and either opioid-antagonist therapy or mechanical ventilation …
The increasing use of buprenorphine as a home-based therapy for opioid addiction in the United States raises public health concerns for the pediatric population.”
The take-home message here is that as drug treatment increases and becomes ever-more prevalent among all age groups, the risk of unintentional exposure increases as well. Toddlers will stick just about anything in their mouth, and young children will often not recognize there’s a difference between pills and candy.
As parents and caregivers, we simply must take the necessary precautions to keep all medications in a safe place, well out of reach of curious hands. Failure to safeguard your medications can have profoundly tragic consequences, so please, do not take this matter lightly.
from Articles https://ift.tt/2vh939u
via IFTTT
Why the Time Is Right for an Inexpensive Bidet
Who wants to talk about poop? Well, unless you’re 5, it’s likely not a daily topic of conversation. But, if you’re constipated, it may be on your mind nearly every minute of the day until you find relief.
Your poop can tell you a lot about your health. Its color, consistency, shape and form are important factors that reveal information about your intestinal health. How often you go is also an indicator. Straining can increase your risk of bowel and pelvic problems, while how you clean up afterward may have an impact on your exposure to pathogens.
On the topic of toilet habits, the clean-up method you use is also important, not just for your health but also for the environment. If you watch any television at all, you’ve likely been convinced that softer toilet paper is better, two-ply is important and the more squares on the roll the better the value. However, more than one pooping principle is needed to keep things moving and sanitary.
Clean Up in Aisle Two
If you were raised in the U.S. you likely grew up using toilet paper and may not be aware of other options. Toilet paper may be standard in the U.S. but it isn’t necessarily the top choice for cleaning yourself after using the restroom. The best way — a bidet (pronounced bih-day) — is used so infrequently by Americans that Trip Savvy1 has dedicated a page to helping travelers who find themselves in a room with an accessory next to the toilet.
There is some debate as to whether the bidet system was started by the French or the Italians.2 But once it was created, the designs became an art form and turned using the bathroom into an “experience.” One of the most well-known bidets was a silver one owned by Napoleon Bonaparte, who traveled with it and willed it to his son.
Dr. Evan Goldstein, a rectal surgeon in New York, spoke with Insider about bidets, saying,3 "Charmin and all these brands have done a great job making us think that toilet paper is hygienic. It's not.”
Those who advocate for the use of bidets say toilet paper does nothing more than smear poop across your backside without cleaning off the pathogens lurking in fecal material. Goldstein compared this to stepping in dog poop and then wiping off the bottom of your shoe, fully expecting all the poop to be gone.4
A bidet works by aiming a small stream of water around your anus to rinse off any material that’s left after you’ve had a bowel movement. There are several styles ranging from simple and inexpensive models that attach to your toilet, to fully automated fixtures with “antimicrobial sanitizing technology and motion-sensing lids.”5
The safety of a bidet is dependent on water pressure and the aim of the product. As you might imagine, men and women may find it uncomfortable — to say the least — if the pressure is high and it’s aimed a little too far forward. Women face a secondary risk of altered vaginal microflora and fecal contamination of the vagina.6
Since many models allow the user to aim the stream, this risk may be mitigated using the same technique women should use with toilet paper, cleaning from front to back to avoid contamination.
The Issue With Tissue Is Virgin Forest Fiber
Some toilet paper may be necessary for patting your bottom dry after using a bidet, but not at the rate Americans are burning through it. CleanTechnica7 reports the average person in the U.S. will use 141 rolls in a year, or roughly 2.7 rolls of paper a week.
With the U.S. Census Bureau8 reporting a current population of 329.2 million, all of whom will likely use toilet paper, it is obvious that tissue is big business. When choosing among the various brands, many people look for variables such as soft, strong and the ease in tearing portions away from the roll.
One variable that isn't often considered is how many mature trees must be cut down so paper can be flushed away. What is cheap and convenient on the store shelves is creating a rising debt the planet is unable to pay.
According to the Natural Resources Defense Council (NRDC),9 most toilet paper products are made from wood pulled from virgin forests in northern Canada. Yet, options exist for manufacturing sustainably produced tissue products using responsibly sourced fibers. The NRDC report revealed:10
"Procter & Gamble, Kimberly-Clark, and Georgia-Pacific use zero recycled content in their at-home toilet paper, instead relying on ancient trees clear-cut from the Canadian boreal forest (the ‘Amazon of the North’)."
Devastation of the environment is causing massive harm to indigenous peoples who call the forest their home. This area where tree harvesting is taking place is also the only place on Earth where certain wildlife species may be found. Virgin forests exist in mature ecosystems without influence from humans. CleanTechnica describes the process of stripping the environment for tissue this way:11
"Trees that sprouted when your great-great-great grandparents were born are chopped down, converted into tissue pulp, rolled into perforated sheets or stuffed into boxes, and flushed or thrown away."
In the NRDC report, they ranked tissue brands for sustainability from A to F. Brands receiving a “D” or “F” included Scott, Angel Soft, Quilted Northern and Charmin. Brands using recycled content received an “A” from NRDC and included:
|
Green Forest |
Seventh Generation |
|
Earth First |
Natural Value |
|
365 Everyday Value, 100% Recycled |
Trader Joe’s Bath Tissue |
Better Bowel Movements Start With Fiber
Choosing the best way to clean yourself after using the restroom isn’t the only concern. Chronic constipation is uncomfortable, sometimes painful, and can lead to more serious health problems such as colorectal cancer12 and chronic kidney disease.13 Constipation doesn't start at the end of the digestive process but, rather, at the beginning. In other words, many times problems with hard-to-pass stools begin with what you eat and drink.
Some of the things that factor into the overall picture include dehydration, lack of fiber, changes to gut microbiota,14 taking certain medications and ignoring the urge to have a bowel movement.15 Lack of fiber and low fluid intake are two of the most frequently overlooked.
Although you might be tempted to reach for a laxative if you struggle with constipation, when those medications are used frequently, they may result in dependency that ultimately exacerbates the issue.16 Instead, focus on your fluid intake and food choices to make a difference.
Processed foods, for instance, have little fiber and they contribute to constipation, so swap them out for whole, raw fruits and vegetables. Processed foods are also high in sugar, which feeds unhealthy gut bacteria and triggers an imbalance that contributes to constipation.17 Foods known to help relieve constipation include leafy greens, avocados, fermented vegetables and prunes.
In addition to eating foods high in fiber, it's important to stay hydrated. While it may be simpler to count the number of glasses of water you drink, it turns out that many foods also have high water content, such as leafy greens and melons.
The best way to determine your hydration status is to look in the toilet after you go to the bathroom. Your urine should be a light-yellow, straw color. This color indicates you have enough fluid in your body to support your kidneys and intestines. As the color of your urine comes closer to amber, it means you're becoming dehydrated.18
Also, don't wait until you’re thirsty to start drinking.19 By the time you feel thirsty you're already dehydrated, which in turn can lead to constipation as your body tries to retain more water by drawing it out of your stool.
Consider Your Potty Posture to Relieve the Pressure
The posture you use on the toilet also has an influence on how easily you can empty your bowels. Most people sit on the toilet to poop but this actually puts your lower intestines in an awkward position, making it hard to fully evacuate. When you sit, your knees are close to a 90-degree angle in relation to your stomach.
In this position the muscle around the neck of the rectum — the puborectalis muscle — tightens and makes it more difficult to pass stool.20 On the other hand, while you're squatting the puborectalis muscle relaxes and the rectum opens more fully, allowing for easier movement.
If you find this conversation uncomfortable, it might be helpful to know even in medical circles discussions about assuming the position to poop has been avoided.21
Changing toilet habits over the years from squatting to sitting has increased the burden of pelvic disease, including bowel disease and pelvic floor injury in women. The authors of one recent study said:22
"To conclude, the porcelain throne has caused unnecessary suffering to many. It also wasted billions of dollars of the countries as health-care costs. The time has come to reacquaint people with their natural habits and put this unfortunate experiment to an end."
As evidence continues to emerge in support of changing your pooping posture, several devices have entered the market to help you achieve a squatting position while sitting on a toilet.
After all, you don't want to give up indoor plumbing and most of us aren't coordinated enough to balance squatting on a toilet seat. One simple device is a foot stool23 that places your body in a more natural position. It is an inexpensive way to improve your posture and virtually anyone can benefit.
Turn and Look Before You Flush
Having a regular bowel movement is important to optimal health and how you feel. If they come too frequently or not often enough it can make you bloated and uncomfortable, interfering with your body's ability to absorb nutrients. However, what's regular for one person may not be regular for another.
Most experts consider anything from three bowels movements a day to three a week as being within a normal range.24 More important than this number is the ease with which you are able to go. It should take no more effort than urinating or passing gas.
Once you've completed your mission it's important to turn around and look. Don't be embarrassed — no one's watching. Your stool is about 75% water25 and the rest is dead bacteria, indigestible food, fats and inorganic matter.
What you see is an indication of how your gastrointestinal tract is functioning. You're evaluating the color, odor, shape, size and even the sound it makes when it hits the water, as well as whether it's a "sinker" or a "floater." The Bristol Stool Chart below was originally published in the Scandinavian Journal of Gastroenterology in 1997 and is a visual representation of what you might find in the toilet.
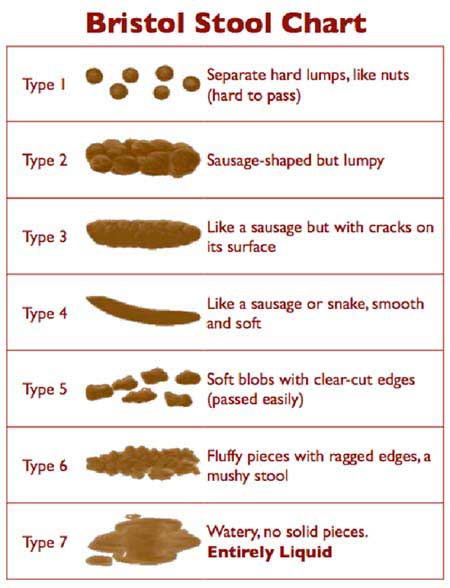
Ideally your stool should be close to Types 3, 4 or 5, with Type 4 generally considered "the Holy Grail" of poop.26 You'll find a list of factors to help you determine what's healthy and what's not at "What Should Your Poop Look Like?" If you have a change in your bowel habit or stool formation with abdominal pain, be sure to seek medical attention.
from Articles https://ift.tt/2HYFJXY
via IFTTT
Top Five Tips to Avoid Dangerous Chemicals
Endocrine-disrupting chemicals (EDCs) are among the most destructive chemicals in our environment. Exposure to them is linked to growth, neurological and learning disabilities, obesity, diabetes, male and female reproductive dysfunction, birth defects, cardiovascular disease and some cancers.1
EDCs are not just harmful — they are also found almost everywhere and hard to avoid. They lurk in food packaging, nonorganic food, nonstick cookware,2 detergents, cosmetics,3 lotions, products with fragrance, antibacterial soaps,4 medicines, toys,5 fabrics, carpets, furniture, construction materials treated with flame retardants, pesticides and more.6
When an endocrine-disrupting chemical exerts permanent and even transgenerational changes to fat cells it is sometimes called an obesogen. Experts believe obesogens encourage the growth of fat cells and fat accumulation through metabolic and appetite alterations that increase the number and size of adipose cells.
Examples of obesogens are bisphenol-A and parabens, and other obesogens may be found in flame retardants, pesticides and other chemicals. But the good news is there are at least five ways you can reduce your exposure to EDCs and obesogens, according to Dr. Leonardo Trasande, who wrote about EDCs for Medscape.
Top Five Tips to Avoid Dangerous Chemicals
Here are my five tips, adapted from Trasande’s article:
1. Beware of certain cookware — Nonstick pans contain perfluoroalkyl substances, or PFAS, chemicals that slow the metabolism rate and cause weight regain.7 Cast iron and stainless steel cookware are good alternatives. Use glass to store your food and reusable storage bags at home and to bring food home from the grocery store.
2. Fight indoor pollution — Flame retardants used in mattresses, carpets, furniture and electronics accumulate in household dust, impairing thyroid function. Open windows and use a wet mop to diminish them. Check if your upholstery has added flame retardants.8
3. Eat organic and avoid canned foods — Organic food is free from GMOs and pesticides, which may disrupt the thyroid, impair cognition and cause cancer.9 Choose grass fed, humanely raised meat and dairy products.
Canned foods may contain bisphenols, which are estrogenic and make fat cells larger. They persist in the environment, double Type 2 diabetes risk and likely pose toxicity to embryos.10 Don't use pesticides on your lawn, and remove shoes when you enter your house.
4. Don't microwave, and avoid packaged goods — A "microwave safe" label is misleading because microscopic polymers break down and get into food.11 Processed and packaged foods contain high fructose corn syrup, artificial sweeteners, pesticides and other obesogens. Phthalates in food packaging and take-out containers can impair lipid and carbohydrate metabolism and increase weight.12
5. Avoid vinyl and plastic — Use a cloth shower curtain that can be machine washed. These stay cleaner and last longer than vinyl. Replace luggage and backpacks with products made of organic blend canvas.
Obesogens and Obesity Are Linked
Obesity has become a worldwide epidemic. Between 1980 and 2010 the rate of obesity in the U.S. doubled and, worldwide, the rate of obesity tripled.13 Obesity in children is especially booming, almost always condemning them to life as obese adults.14 Obesity, because of its association with Type 2 diabetes, cancer and cardiovascular disease, costs the U.S. approximately $200 billion a year.
The common belief that increased caloric consumption and reduced exercise cause the obesity epidemic does not explain the phenomenon, says research in the journal Basic & Clinical Pharmacology & Toxicology. Rather, people may be predisposed to obesity from exposure to obesogens in the womb, write the researchers.15
"Adult mice exposed to TBT [tributyltin, an obesogen] in utero displayed increased lipid accumulation in adipose depots, livers and testis and treatment of adolescent or adult mice, rats, goldfish and zebrafish led to increased fat deposition and hepatic steatosis ...
TBT continues to be found in house dust and in seafood, and at least one study shows increased ponderal index in human infants with the highest prenatal TBT exposure."
Other chemicals have similar effects, write the researchers, such as the fungicides triflumizole and tolylfluanid and the plasticizer diethylhexyl phthalate.16 Obesogens do not just increase the fat levels immediately seen in test animals: The fat augmentation properties may persist for generations, the researchers write.17
"Prenatal exposure to environmental obesogens can produce lasting effects on the exposed animals and their offspring to at least the F4 generation. Recent results show that some of these transgenerational effects of obesogen exposure can be carried across the generations via alterations in chromatin structure and accessibility."
Apparently, obesogens not only can program organisms to accumulate fat; they can program their offspring to do the same.
What Causes the Fat Accumulation to Occur?
Researchers note in Basic & Clinical Pharmacology & Toxicology that cells exposed to an obesogen did not accumulate more fat than unexposed cells but differ in another way: they "did not respond to normal signalling processes." Specifically, write the researchers, the cells:18
" … expressed reduced levels of GLUT4 accompanied by lower glucose uptake. They produced lower levels of adiponectin mRNA and protein and showed elevated levels of molecular markers of inflammation and fibrosis. The ... cells were impaired in their respiratory function, measured in vitro and, as might be expected, contained fewer mitochondria."
Like the research in Basic & Clinical Pharmacology & Toxicology Research, a paper in Pediatric Research seems to confirm that obesogenic effects are seen transgenerationally. Fetal exposure to phthalates, which are obesogenic, is correlated with obesity in the exposed children, write the researchers.19
"Higher concentrations of urinary MEP, MBzP, and ΣDEHP [phthalates] metabolites in pregnant mothers were associated with increased odds of their children being overweight or obese ...
Higher prenatal MEP concentrations were consistently associated with increased BMI, waist circumference, and percent body fat in children between 5 and 12 years of age … onset of puberty did not affect our findings. In addition, unlike previous studies, our results were quite similar between boys and girls."
There Are More Obesity Links to Obesogens
Perfluoroalkyl substances, or PFASs, which are endocrine-disrupting chemicals that are obesogenic, have also been linked to obesity in the scientific literature. A 2018 study in PLOS Medicine found:20
"In this diet-induced weight-loss trial, higher baseline plasma PFAS concentrations were associated with a greater weight regain, especially in women, possibly explained by a slower regression of RMR [resting metabolic rate] levels.
These data illustrate a potential novel pathway through which PFASs interfere with human body weight regulation and metabolism. The possible impact of environmental chemicals on the obesity epidemic therefore deserves attention."
A 2018 study in Environmental Research on the exposure of pregnant women to phthalates also concluded:21
"Exposure to certain phthalates during pregnancy may be associated with long-term weight change in women. More studies on the effects of phthalate exposure during pregnancy on women's long-term health are required."
Endocrine Disrupting Chemicals Linked to Diabetes
Diabetes is a major public health concern in the U.S. and other countries and endocrine disrupting chemicals contribute to the problem. Research in the journal Environmental Health Perspective finds "positive associations between exposure to BPA and BPS and the incidence of Type 2 diabetes, independent of traditional diabetes risk factors."22
Bisphenol A (BPA) and bisphenol S (BPS) are common EDCs. BPA is found in polycarbonate plastic and many canned foods, and metal jar lids have BPA in their linings.23 BPS, a BPA analogue, was thought to be safer than BPA, but research now reveals the two have similar risk profiles.24 Researchers in Environmental Health Perspectives wrote:25
"This study is one of the few prospective studies on the association between exposure to BPA and the subsequent development of type 2 diabetes and the first one on diabetes that relies on repeated urinary bisphenols measurements to assess exposure, which is crucial given the short half-life of BPA in the body.
To the best of our knowledge, this is also the first study to investigate exposure to BPS in relation with the risk of developing diabetes. Our results suggest associations between diabetes risk and both BPA concentrations and BPS detection in urine."
Research in rats that was published in Environmental Health Perspectives in 2017 apparently duplicates the EDC and diabetes findings.26
"Overall summary estimates indicated significant positive associations between BPA and fat weight ... Findings from our systematic review suggest that early-life exposure to BPA may increase adiposity and circulating lipid levels in rodents ...
It is important to note that although this review focused on BPA, other chemicals with putative obesogenic effects have also been identified.
For instance, the BPA analog bisphenol S and several other chemical classes have been identified as potential obesogenic chemicals; these include phthalates, organotins, perfluorinated alkyl acids, brominated flame retardants, (non)-dioxin-like polychlorinated biphenyls, and several pesticides."
The Endocrine Society Also Questions EDC Safety
The Endocrine Society, the world’s largest organization of endocrine clinicians and scientists, has also researched the risks of endocrine disrupting chemicals. The society says it:27
"defines an endocrine-disrupting chemical (EDC) as 'an exogenous chemical, or mixture of chemicals, that can interfere with any aspect of hormone action' ...
EDCs are found in many different products, including plasticizers, personal care products, and pesticides. Furthermore, EDCs such as polychlorinated biphenyls (PCBs) and dioxins are found in environmental contaminants.
Humans are constantly exposed to EDCs on a daily basis by ingestion, inhalation, and dermal contact, and with this constant exposure has come detrimental effects on reproductive health.
Specifically, EDCs are known to decrease fertility in both male and female animal models and they are associated with subfertility/infertility in humans.
These chemicals can affect the production of steroids (steroidogenesis), ovarian follicle development and growth (folliculogenesis), and development and maturation of sperm (spermatogenesis), leading to complications with reproduction."
Toxic Chemicals Are Everywhere
Toxic chemicals are all around; in your food, water, air and countless commonly used products and goods, and this onslaught is having a definitive effect — even when exposures are relatively low. Yes, plastics have made modern life more "convenient" but the harm they cause is not worth it. The dangers are especially pronounced during pregnancy and early infancy.
The idea that chemicals affect your health should come as no surprise. What may be surprising is the extent of your exposure. Most of us go about our day, touching, eating, drinking and breathing with few concerns about what we’re actually coming into contact with.
As you saw above in the different scientific studies, the obesogenic effects of EDCs are especially clear, causing obesity and other metabolic problems. Obesity, in turn, is linked to other diseases like diabetes, high blood pressure and certain cancers.28 But the damage from EDCs and obesogens can be reduced through commonsense lifestyle choices.
from Articles https://ift.tt/37Wzoah
via IFTTT