Health, Fitness,Dite plan, health tips,athletic club,crunch fitness,fitness studio,lose weight,fitness world,mens health,aerobic,personal trainer,lifetime fitness,nutrition,workout,fitness first,weight loss,how to lose weight,exercise,24 hour fitness,
Labels
Technology
New Post
Microbes in the gut could be protective against hazardous radiation exposure
from Top Health News -- ScienceDaily https://ift.tt/3jPmuR3
The Case Against Processed Vegetable Oils
Dr. Paul Saladino is the author of “The Carnivore Code.” I’ve previously interviewed him about the carnivore diet and the impact of metabolic health on COVID-19 outcomes. The video1 above features Saladino on a recent episode of the Joe Rogan podcast.
It’s a three-hour conversation, but my focus here is on Saladino’s viewpoints on omega-6 seed oils, and the surprising fact that conventional chicken and pork are significant stealth sources of oxidized omega-6 fats that can contribute to ill health by impairing vital mitochondrial signaling.
Vegetable Oils Are Responsible for Epidemic of Ill Health
In recent years, it’s become increasingly clear that one of the most damaging components in our modern diet is processed vegetable oils, as they contain excessive amounts of oxidized omega-6 linoleic acid, a polyunsaturated fat (PUFA). The biological damage they cause is even worse than that caused by refined sugar and high fructose corn syrup.
According to ophthalmologist Dr. Chris Knobbe, who has researched the matter extensively, virtually all chronic metabolic and degenerative diseases, including age-related macular degeneration, are primarily caused by a preponderance of industrial vegetable oils in the diet.
The reason for this is because these oils trigger mitochondrial dysfunction that then drives the disease process, and several studies2,3,4,5,6,7,8 have demonstrated the truth of this. The good news is that simply replacing dangerous oils with healthy saturated fats can go a long way toward boosting your health and reducing your risk of chronic disease.
Unfortunately, many health authorities have insisted — and still insist — omega-6-rich oils like soybean, corn and canola oil are healthier than saturated animal fats such as butter and lard, and this myth has been a tough one to dismantle, despite the evidence against it.
How Processed Vegetable Oils Harm Your Health
There are many reasons to avoid or eliminate industrially processed seed oils from your diet. As mentioned, vegetable oils are a concentrated source of omega-6 linoleic acid, which can lead to a severe imbalance between the omega-6 to omega-3 ratio in your diet.
In fact, I’ve found it is extremely difficult to correct this imbalance simply by taking more omega-3. In fact, excess omega-3 can also contribute to ill health. Your first and most important step is to cut down on the omega-6s, or else you’re always going to be nutritionally lopsided.
Even organic, biodynamic olive oil can shift your ratio in the wrong direction, as olive oil is also a source of omega-6 linoleic acid. If, like me, you’re in the habit of eating olive oil, you may want to limit your intake to 1 tablespoon per day or less. The problem, really, is twofold:
- Most people get far too much omega-6 and too little omega-3, thus ending up with a lopsided ratio, and this ratio is what impacts health. Ideally, this ratio would be close to 1-to-1
- Most of the omega-6 people eat has been damaged and oxidized through processing
Then there’s the issue of direct toxicity from pesticides and herbicides. Most of the vegetable oils produced today — especially canola, corn and soy — are made from genetically engineered (GE) crops, and are therefore a significant source of toxic glyphosate exposure.
Thirdly, vegetable oils degrade to extremely toxic oxidation products when heated, including 4-hydroxynonenal (4HNE) cyclic aldehydes,9 which are what cause oxidized low-density lipoprotein (LDL) associated with heart disease. Aldehydes also crosslink tau protein and create neurofibrillary tangles, thereby contributing to the development of neurodegenerative diseases. Processed vegetable oils also harm health by:
|
Increasing inflammation.10 |
|
Damaging the endothelium (the cells lining your blood vessels) and causing an increase in penetration of LDL and very low-density lipoprotein (VLDL) particles into the subendothelium. In other words, these oils get integrated in your cell and mitochondrial membranes, and once these membranes are impaired, it sets the stage for all sorts of health problems. As discussed in my July 2020 interview with Knobbe, the PUFAs from vegetable oils, seed oils and trans fats are primarily stored in your fat cells, opposed to being used for fuel, and have a half-life of 600 to 680 days.11 They also get incorporated into tissues, including your heart and brain. One result of this could be memory impairment and increased risk of Alzheimer’s disease, which is exactly what they found with canola oil.12 As reported in one 2017 study:13
|
|
Damaging your mitochondria and DNA by making your cell membranes more permeable, allowing things to enter that shouldn’t. |
|
Making the cell membrane less fluid, which impacts hormone transporters in the cell membrane and slows your metabolic rate. |
|
Inhibiting cardiolipin, an important component of the inner membrane of your mitochondria that needs to be saturated in the omega-3 fat DHA to function properly. Cardiolipin can be likened to a cellular alarm system that triggers apoptosis (cell death) by signaling caspase-3 when something goes wrong with the cell. If the cardiolipin is not saturated with DHA, it cannot signal caspase-3, and hence apoptosis does not occur. As a result, dysfunctional cells are allowed to continue to grow, which can turn into a cancerous cell. |
|
Inhibiting the removal of senescent cells, i.e., aged, damaged or crippled cells that have lost the ability to reproduce and produce inflammatory cytokines that rapidly accelerate disease and aging. |
|
Stripping your liver of glutathione (which produces antioxidant enzymes), thereby lowering your antioxidant defenses.14 |
|
Inhibiting delta-6 desaturase (delta-6), an enzyme involved in the conversion of short-chained omega-3s to longer chained omega-3s in your liver.15 |
|
Exposing you to toxic 4-hydroxynonenal (4HNE), which forms during the processing of most vegetable oils, even if the oil is obtained from organic crops — 4HNE is highly toxic, especially to your gut bacteria, and consumption of 4HNE has been correlated with having an obesogenic balance of gut flora. It also causes DNA damage and instigates free radical cascades that damage your mitochondrial membranes.16 |
The Molecular Biology of PUFAs
If you want to go deep and geek out on the molecular biology of what is going on with excessive linoleic acid (LA) intake, then I strongly advise watching the video above.
Saladino interviews veterinarian Peter Dobromylskyj, who maintains the Hyperlipid Blog.17 In it, they describe in great detail how eating these seed oils and other foods high in LA, like chicken and pork, destroy mitochondrial signaling in the adipocyte and disrupt your metabolic functioning.
One key point from this Dobromylskyj interview is the explanation of how PUFAs break your metabolic mechanism and contribute to obesity. As explained by Saladino, as he reviews a study on this topic:
“Let’s look at what happens when you give humans a bunch of polyunsaturated fats … You are supposed to be insulin resistant in ketosis. That’s how your body partitions glucose to the cells that need it.
And here you have a ketogenic diet based on … canola oil, safflower oil or soybean oil, and you see people remain insulin sensitive when they’re in ketosis. This is clear evidence that polyunsaturated fats are breaking your metabolism. Glucose is lower because it’s going into your cells; it’s making bigger cells. You’re getting fat.”
For clarity, does this mean a ketogenic diet, meaning a diet high in healthy fats and low in non-vegetable carbs, is fattening? No. The take-home message here is that a proper ketogenic diet must be based on healthy saturated fats, not destructive vegetable seed oils that are loaded with LA.
Eating a high-fat diet, when the fats are primarily LA from processed vegetable and seed oils, is far worse than eating a chronic high-carb diet. The type of fat is of crucial importance, as it impacts your mitochondrial, cellular and metabolic functioning.
Fats like LA can persist in your cell membranes for months to years, continuing to wreak havoc with your metabolism the entire time, while the sugar is quickly metabolized.
Aside from that, this also helps explain why processed foods are so fattening. It’s not just that they’re loaded with added sugars. They’re also loaded with LA that breaks your metabolic machinery and promotes fat accumulation and inflammation.
Choose Your Fats Carefully
Examples of healthy fats that belong in your diet include but are not limited to organic coconut oil, ghee, grass fed butter, lard, tallow, black seed oil (Nigella sativa), avocados, raw dairy products, olives, organic pastured eggs and raw nuts.
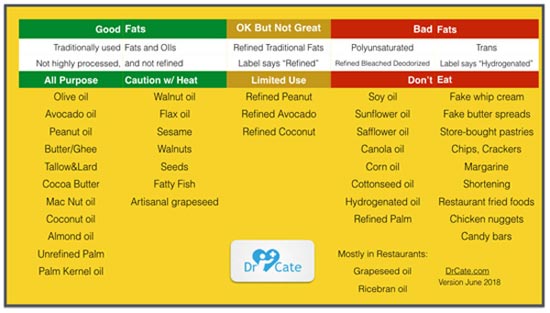
To learn more about the ins and outs of dietary fats, pick up a copy of my book “Superfuel: Ketogenic Keys to Unlock the Secrets of Good Fats, Bad Fats, and Great Health,” cowritten with James DiNicolantonio, Pharm.D., which gives more in-depth specifics on how to discriminate between healthy and harmful dietary fats. Dr. Catherine Shanahan’s list of good and bad cooking oils and fats is also useful.
Stealth Sources of Harmful PUFAs: Chicken and Pork
As explained by Saladino in the featured Rogan interview, aside from processed foods (which are loaded with vegetable oils) and vegetable cooking oils, there are also two common stealth sources of harmful PUFAs in the modern diet, namely conventionally farmed chicken and pork.
He shows a graph illustrating meat consumption, which has significantly risen over the decades. But it’s not the total consumption that is causing the problem, he notes. Specifically, the problem is not related to red meat consumption, which has actually gone down. Rather, it’s “lean white” meats, particularly chicken but also pork, that help drive the chronic disease trend.
Long thought of as a healthier type of meat, primarily because it’s leaner than red meat, the problem with conventional chicken (and pork) is that the animals are fed corn — typically GE varieties that are farmed with glyphosate.
And what happens when animals are fed corn? The meat becomes high in omega-6 linoleic acid, as corn is high in this type of fat.18 So, as Saladino points out, high chicken consumption actually adds to your vegetable oil consumption, and can therefore contribute to systemic inflammation, mitochondrial dysfunction and metabolic ill health.
“PUFAs act differently in our body,” Saladino says in the Rogan interview. “At the level of our mitochondria, it looks like this polyunsaturated fat, this linoleic acid-rich vegetable oil, is signaling things differently.
There’s a lot of compelling evidence to suggest linoleic acid is driving adipocyte hypertrophy — the fat cells are getting bigger. Fat cells can do two things. They can get bigger or they can divide. When fat cells get big, and don’t divide, they eventually start leaking inflammatory mediators.”
This doesn’t mean you cannot eat chicken or pork. However, unlike cows, buffalo and lambs, these animals have only one stomach and as such any omega-6 fats they eat are not metabolized and stored in their tissues. Since these animals, even healthy organically grown animals, are typically fed grains, they are loaded with omega-6 fats and may have 10 TIMES the LA content that beef, lamb or buffalo do.
That is why I think it is really a good strategy to avoid eating these meats and replace them with animals which have far lower LA content. If you want to know how much LA you are eating simply go to cronometer.com and carefully enter your food that is accurately weighed out and you can see precisely how much LA you are eating. It would be great to get your daily intake under 10 grams per day.
Safeguard Your Health by Ditching Vegetable Oils
To recap, if you want to avoid dangerous fats of all kinds, your best bet is to significantly reduce or eliminate the following from your diet:
- Processed foods of all kinds
- Industrially processed cooking oils such as corn oil, canola oil, soy and cottonseed oils
- Conventionally farmed chicken
- Conventionally farmed pork
My comprehensive nutrition plan offers helpful guidance for this process. When cooking, coconut oil, butter, lard and ghee are healthy options. Also be sure to swap out margarines and vegetable oil spreads for organic butter, preferably made from raw grass fed milk. Butter is a healthy whole food that has received an unwarranted bad rap.
To further balance your omega-3 to omega-6 ratio you may also need a high-quality source of animal-based omega-3 fat, such as krill oil, if you’re not in the habit of eating small, fatty fish such as sardines, anchovies and mackerel, and/or wild caught Alaskan salmon.
from Articles https://ift.tt/3mFk2Pa
via IFTTT
What Are Long-Term Health Effects of Daylight Saving Time?
Twice each year, every U.S. state except Hawaii and Arizona transition from daylight saving time (DST) to standard time and back again.1 Yet, the research is quite clear that meddling with time, and therefore sleep, has negative effects on your health.
DST was first introduced in 1918 when it was called "fast time."2 The law was signed by the president to support the war effort. It followed a similar initiative in Germany that went into effect in 1916.3 After the war ended, the law was repealed and then reinstated during World War II.4 Three weeks after World War II ended, the law was again repealed.
By 1963, Time magazine called the resulting state of confusion a "chaos of clocks."5 Nearly 20 years after the end of World War II, DST was restored under the Uniform Time Act.6 This standardized when DST would begin and end, and gave states the option to stay on standard time year-round.
In 1973, Congress determined DST should be observed all year, but this was again changed in 1974 when the clocks were moved forward in the spring and fell back an hour in the fall.7 In 1986 the time officially changed at 2 a.m. on the first Sunday in April and the last Sunday in October.
The date in the fall changed in 2005 to the first Sunday in November in response to lobbying from the golf, barbecue and candy companies, which wanted more daylight during the evening hours to accommodate Halloween night and the traditional passing of sugar treats.8 The current dates and times have remained unchanged since 2007.
Long-Term Health Effects of Daylight Saving Time
Part of the risk posed by DST is that it can shrink the average amount of sleep an adult gets by up to 20 minutes during transitions.9 Chronic sleep disruption contributes to a rising number of people who are obese.10 Dr. Chris Winter, author of "The Sleep Solution: Why Your Sleep Is Broken and How to Fix It," explains how sleep is an integral part of your eating patterns by affecting the hormones ghrelin and leptin:11
"Appetite in general is often not the body requesting food; it's the body anticipating food. When your body knows you eat lunch around 12:30 p.m. or so every day, it anticipates and prepares for the meal.
These two hormones are intimately associated with sleep, which is part of why when we're not sleeping well, we tend to overeat. It's a tight hormonal balance and daylight-saving shifts can absolutely throw it off."
A lack of sleep may also raise the risk you can experience a fatal accident. Dr. Beth Ann Malow from Vanderbilt University Medical Center and colleagues published a commentary reviewing large epidemiological studies that document these negative health effects.12 Malow commented on their findings:13
"People think the one-hour transition is no big deal, that they can get over this in a day, but what they don't realize is their biological clock is out of sync. It's not one hour twice a year. It's a misalignment of our biologic clocks for eight months of the year.
When we talk about DST and the relationship to light, we are talking about profound impacts on the biological clock, which is a structure rooted in the brain. It impacts brain functions such as energy levels and alertness."
Another team of researchers published an analysis of the effect daylight saving time has on a spectrum of diseases.14 They gathered data using a population-based, cross-sectional analysis from an insurance claim data set of over 129 million patients in the U.S. and Sweden.
They evaluated the effect shifting time by one hour twice each year had on hundreds of age- and sex-specific health conditions. Their data confirmed past research results that heart attacks,15 accidents,16 mental health concerns17 and immune-related diseases18 increase during the time shift.
The analysis also revealed several surprises. For instance, it showed an increase in substance abuse in men ages 41 to 60 near DST.19 They also found immune-related disorders that had not been associated in the past with daylight saving time occur more often in the first week following the spring DST shift.
The analyses revealed a higher number of complications during pregnancy and childbirth, and increases in renal failure.20
"To the best of our knowledge, we are the first to report the DST-related RRs [relative risk] of disorders involving the digestive system (such as noninfective enteritis and colitis), which rose three percent after the spring DST shift in females over 60 and six percent in males under ten."
Your Suprachiasmatic Nucleus Is Involved
Your body runs on an internal clock known as your circadian rhythm. When you mess up this internal clock, your cells are exposed to an unusual amount of stress. Many of the health conditions attributed to the biannual time change are because these internal clocks are not easily reprogrammed and are synchronized to a 24-hour cycle of light and dark.21
Another system in the body responsible for regulating your internal clock is located in the hypothalamus and called the suprachiasmatic nucleus (SCN).22 It functions through hormonal and chemical signals to synchronize your internal clock, which in turn regulates your sleep-wake cycle and has an effect on the regulation of other physiological activities.
These activities include your core body temperature, neuroendocrine function, memory and psychomotor activity.23 The SCN is made up of multiple circadian oscillator neurons that function a little like a pacemaker.
Although your body uses several environmental cues to regulate your circadian rhythm, the most important is your exposure to light. Your SCN produces an electrical output using a specific rhythm in response to light.24 Aging and sleep deprivation will have a negative effect on the electrical amplitude of your SCN, which is essential for optimal behavioral and physiological mechanisms.
There's growing evidence suggesting your SCN contributes to cognitive performance and overall health. When there's a negative impact on this 24-hour rhythm it increases your risk for depression, sleep disorders, neurodegenerative disease and cancer.25
Since your SCN responds to light, disruption in light exposure can trigger negative health effects. As the Earth rotates, your body clock adjusts to light changes, including seasonal change.26
However, the sudden adjustments that come with time changes in the spring and fall are what researchers believe triggers the increased incidence of heart attack, stroke, traffic accidents and a higher number of injuries.
Fred Turek from Northwestern University directs the Center for Sleep and Circadian Biology and says this about a one-hour time change twice a year: "You might not think that a one-hour change is a lot. But it turns out that the master clock in our brain is pretty hard-wired."27
Data Don't Support Daylight Saving Time
One of the reasons given for keeping DST, despite strong evidence it has negative health effects, is the potential it may help save energy. However, as this short video demonstrates, while it may have originally reduced energy use in the early 1900s, the cost difference for a single-family in modern times is just $4 each year.
A second argument is that it offers people more sunlight after work to enjoy recreational activities. Theoretically, this may lead to more physical activity and better health. However, a study published in 2014,28 which gathered data from people living in Colorado, Utah, New Mexico and Arizona, found it did not make a difference in the amount of time outdoors, but had an effect on the types of activities.
They concluded, "… the potential for DST to serve as a broad-based intervention that encourages greater sports/recreation participation is not supported by this analysis."
Financial losses are also felt in the stock market. An analysis published in the American Economic Review revealed each time the clocks changed there was an impact on the function of the financial markets.29 The scientists believe desynchronized sleep reasonably explained the effect on the market that was different from other Mondays on the two weekends when the time changes.
When a potential $4 savings in energy is compared against the loss of finances, productivity and rising health care costs from injuries and illness, it's apparent moving the clocks in the spring and the fall is not an effective way of managing human and environmental resources.
Experts also disagree about how long it takes your body to recover from the time change. Till Roenneberg is a German chronobiologist who says his studies demonstrate your body's circadian clock never adjusts during DST. In an interview with a reporter from National Geographic, he said:30
"The consequence of that is that the majority of the population has drastically decreased productivity, decreased quality of life, increasing susceptibility to illness, and is just plain tired. Light doesn't do the same things to the body in the morning and the evening. More light in the morning would advance the body clock, and that would be good. But more light in the evening would even further delay the body clock."
Europe Is Ditching DST in 2021
Many Europeans will soon not have to struggle with a biannual time change. March 26, 2019, the European Parliament voted to end DST in 2021.31 The Guardian reported that member states will be allowed to "choose whether to remain on 'permanent summer' or 'permanent winter' time under the draft directive."32
Europeans call DST "summertime" and standard time is "wintertime." This means countries that opted to remain permanently on summertime will make their final adjustments in March 2021. Countries that decide to remain on permanent wintertime will change their clocks for the last time in October 2021.
As more published data establish the negative effects on health, finances and productivity, the tide is beginning to turn in the U.S. with state bills introduced each year that propose changes to DST.33
Tips to Transition When the Clock 'Falls Back'
Until DST is either repealed or remains in place year-round, you'll have to make changes to your sleep schedule twice a year. In this short video I share several strategies to help you fall asleep and to improve the quality of your sleep.
Small shifts in your circadian timing are happening all year since many ignore their body's internal clock, either by necessity to accommodate their work schedule or by choice.
Pushing the limit of your body clock by getting up early and staying up late may not be worth it when it comes to your long-term health. University of Alabama associate professor Martin Young has suggested several natural strategies to help resync your body after a time change, including:34
- Wake up 30 minutes earlier on Saturday and Sunday, to minimize the impact of getting up earlier on Monday morning
- Go outside in the sunlight in the early morning
- Exercise in the mornings over the weekend, in keeping with your overall level of health and fitness
- Consider setting your clock ahead on Friday evening, allowing an extra day to adjust over the weekend
I would also add to these recommendations the suggestions from the video above and the following:
- Practice good sleep hygiene, including sleeping in complete darkness, checking your bedroom for electromagnetic fields and keeping your bedroom temperature cool enough for optimal sleep. For a full report about how to maximize the quality of your sleep, see "Sleep — Why You Need It and 50 Ways to Improve It."
- Optimize your vitamin D level to support your immune function, which is especially important during cold and flu season.
- Manage your stress with whatever stress-busting techniques work for you. Consider using yoga, exercise, meditation or Emotional Freedom Techniques.
- Eat dinner earlier and pay attention to your diet, making sure you are consuming plenty of fresh, whole foods, preferably organic, and minimal amounts of processed foods and fast foods; keep your sugar consumption low, especially fructose. I invite you to review our optimized nutrition plan to help you develop an eating plan that supports your overall health.
- Consider encouraging your legislature to change DST by signing a petition to your congresspersons or getting involved in your state to pass a resolution.
from Articles https://ift.tt/35StLur
via IFTTT