Health, Fitness,Dite plan, health tips,athletic club,crunch fitness,fitness studio,lose weight,fitness world,mens health,aerobic,personal trainer,lifetime fitness,nutrition,workout,fitness first,weight loss,how to lose weight,exercise,24 hour fitness,
Labels
Technology
New Post
Statins Double Risk of Dementia, Are Linked to COVID Deaths
The use of statin cholesterol-lowering medications has been on the rise for decades1 and they are among the most widely used drugs in the world. In the U.S., close to 50% of U.S. adults over 75 years old take a statin2 to lower their cholesterol in the misguided hope of preventing heart disease, heart attacks and stroke.
Not only is there strong evidence suggesting that statins are a colossal waste of money, but their use may also harm your brain health — more than doubling your risk of dementia in some cases.3
The benefit must clearly outweigh the risk when it comes to any drug treatment, but this is rarely the case with statins, which do not protect against cardiovascular disease and are linked to a number of health conditions4,5 including dementia, diabetes6 and even increased risk of death from COVID-19.7
Statins Doubled Risk of Developing Dementia
Statins’ effects on cognitive performance have previously been called into question, since lower levels of low-density lipoprotein (LDL) cholesterol are linked to a higher risk of dementia.8 The featured study, published in The Journal of Nuclear Medicine,9 involved people with mild cognitive impairment and looked into the effects of two types of statins: hydrophilic and lipophilic.
Hydrophilic statins, which include pravastatin (Pravachol) and rosuvastatin (Crestor), dissolve more readily in water, while lipophilic statins, such as atorvastatin (Lipitor), simvastatin (Zocor), Fluvastatin (Lescol), and lovastatin (Altoprev), dissolve more readily in fats.10 Lipophilic statins can easily enter cells11 and be distributed throughout your body, whereas hydrophilic statins focus on the liver.12
According to study author Prasanna Padmanabham of the University of California, Los Angeles, “There have been many conflicting studies on the effects of statin drugs on cognition. While some claim that statins protect users against dementia, others assert that they accelerate the development of dementia. Our study aimed to clarify the relationship between statin use and subject’s long-term cognitive trajectory.”13
Subjects were divided into groups based on cognitive status, cholesterol levels and type of statin used, and followed for eight years. Those with early mild cognitive impairment and low to moderate cholesterol levels at the start of the study who used lipophilic statins had more than double the risk of dementia compared to those who did not use statins.14
Further, this group also had significant decline in metabolism of the brain’s posterior cingulate cortex, which is the brain region that declines most significantly in early Alzheimer’s disease.15
Your Brain Needs Cholesterol
About 25% to 30% of your body’s total cholesterol is found in your brain, where it is an essential part of neurons. In your brain, cholesterol helps develop and maintain the plasticity and function of your neurons,16 and data from the Shanghai Aging Study revealed that high levels of LDL cholesterol are inversely associated with dementia in those aged 50 years and over.
“High level of LDL-C may be considered as a potential protective factor against cognition decline,” the researchers noted.17 They compiled a number of mechanisms on why lower cholesterol may be damaging for brain health, including the fact that lower cholesterol is linked with higher mortality in the elderly and may occur alongside malnutrition and chronic diseases, including cancer. As it specifically relates to brain health, however, they suggested:18
- Decreasing cholesterol levels in the elderly may be associated with cerebral atrophy, which occurs with dementia
- High LDL cholesterol may be beneficial by reducing neurons’ impairments or helping repair injured neurons
- Acceleration of neurodegeneration has occurred when neurons were short on cellular cholesterol or cholesterol supply
- Cholesterol plays an important role in the synthesis, transportation and metabolism of steroid hormones and lipid-soluble vitamins, and both of these are important to synaptic integrity and neurotransmission
Lower cholesterol levels were also associated with worse cognitive function among South Korean study participants aged 65 and over, and were considered to be a “state marker for AD [Alzheimer’s disease].”19
A U.S. study of more than 4,300 Medicare recipients aged 65 and over also revealed that higher levels of total cholesterol were associated with a decreased risk of Alzheimer’s disease, even after adjusting for cardiovascular risk factors and other related variables.20
Statins Increase Death Risk From COVID-19
The risks to brain health are only one red flag tied to statins. A concerning link was also uncovered among statins, diabetes and an increased risk of severe disease from COVID-19.21 Among patients with Type 2 diabetes admitted to a hospital for COVID-19, those taking statins had significantly higher mortality rates from COVID-19 within seven days and 28 days compared to those not taking the drugs.
The researchers acknowledged those taking statins were older, more frequently male and often had more comorbidities, including high blood pressure, heart failure and complications of diabetes. However, despite the limitations, the researchers found enough evidence in the over 2,400 participants to conclude:22
“… our present results do not support the hypothesis of a protective role of routine statin use against COVID-19, at least not in hospitalized patients with T2DM (Type 2 diabetes mellitus).
Indeed, the potentially deleterious effects of routine statin treatment on COVID-19-related mortality demands further investigation and, as recently highlighted, only appropriately designed and powered randomized controlled trials will be able to properly address this important issue.”
Statins Double — or Triple — Diabetes Risk
A connection already exists between statins and diabetes, to the extent that people who take statins are more than twice as likely to be diagnosed with diabetes than those who do not, and those who take the drugs for longer than two years have more than triple the risk.23,24
“The fact that increased duration of statin use was associated with an increased risk of diabetes — something we call a dose-dependent relationship — makes us think that this is likely a causal relationship,” study author Victoria Zigmont, a graduate researcher in public health at The Ohio State University in Columbus, said in a news release.25
The data also indicated that individuals taking statin medications had a 6.5% increased risk of high blood sugar as measured by hemoglobin A1c value,26 which is an average level of blood sugar measuring the past 60 to 90 days.
Researchers with the Erasmus Medical Center in The Netherlands also analyzed data from more than 9,500 patients, finding those who had ever used statins had a 38% higher risk of Type 2 diabetes, with the risk being higher in those with impaired glucose homeostasis and those who were overweight or obese.27
The researchers concluded, “Individuals using statins may be at higher risk for hyperglycemia, insulin resistance and eventually Type 2 diabetes. Rigorous preventive strategies such as glucose control and weight reduction in patients when initiating statin therapy might help minimize the risk of diabetes.”
But a far better strategy may be preventing insulin resistance in the first place, by avoiding statin drugs and eating a healthy diet. According to Dr. Aseem Malhotra, an interventional cardiologist consultant in London, U.K. — who has been attacked for being a “statin denier” after calling out the drugs’ side effects28 — and a colleague:29
“In young adults, preventing insulin resistance could prevent 42% of myocardial infarctions, a larger reduction than correcting hypertension (36 %), low high-density lipoprotein cholesterol (HDL-C) (31 %), body mass index (BMI) (21 %) or LDL-C (16 %).30
It is plausible that the small benefits of statins in the prevention of CVD come from pleiotropic effects which are independent of LDL-lowering. The focus in primary prevention should therefore be on foods and food groups that have a proven benefit in reducing hard endpoints and mortality.”
The Statin Scam
Even as saturated fats and cholesterol have been vilified, and statin drugs have become among the most widely prescribed medications worldwide, heart disease remains a top killer.31 Today, statin drugs to reduce cholesterol levels are recommended for four broad patient populations:32
- Those who have already had a cardiovascular event
- Adults with diabetes
- Individuals with LDL cholesterol levels ≥190 mg/dL
- Individuals with an estimated 10-year cardiovascular risk ≥7.5% (based on an algorithm that uses your age, gender, blood pressure, total cholesterol, high density lipoproteins (HDL), race and history of diabetes to predict the likelihood you'll experience a heart attack in the coming 10 years)
Despite statins being prescribed for these sizable groups, and “target” cholesterol levels being achieved, a systematic review of 35 randomized, controlled trials found that no additional benefits were gained. According to an analysis in BMJ Evidence-Based Medicine:33
“Recommending cholesterol lowering treatment based on estimated cardiovascular risk fails to identify many high-risk patients and may lead to unnecessary treatment of low-risk individuals. The negative results of numerous cholesterol lowering randomized controlled trials call into question the validity of using low density lipoprotein cholesterol as a surrogate target for the prevention of cardiovascular disease.”
Even in the case of recurrent cardiovascular events, despite the increase in statin use from 1999 to 2013, researchers writing in BMC Cardiovascular Disorders noted, “there was only a small decrease in the incidence of recurrent CVD, and this occurred mainly in older patients without statins prescribed.”34
Statins Won’t Protect Your Heart Health
Statins are effective at lowering cholesterol, but whether this is the panacea for helping you avoid heart disease and extend your lifespan is a topic of heated debate. Again in 2018, a scientific review presented substantial evidence that high LDL and total cholesterol are not an indication of heart disease risk, and that statin treatment is of doubtful benefit as a form of primary prevention for this reason.35
In short, these drugs have done nothing to derail the rising trend of heart disease, while putting users at increased risk of health conditions like diabetes, dementia and others, such as:
- Cancer36
- Cataracts37
- Triple risk of coronary artery and aortic artery calcification38
- Musculoskeletal disorders, including myalgia, muscle weakness, muscle cramps, rhabdomyolysis and autoimmune muscle disease39
- Depression40
In the event you’re taking statins, be aware that they deplete your body of coenzyme Q10 (CoQ10) and inhibit the synthesis of vitamin K2. The risks of CoQ10 depletion can be somewhat offset by taking a Coenzyme Q10 supplement or, if you're over 40, its reduced form ubiquinol. But ultimately, if you’re looking to protect both your brain and heart health, avoiding statin drugs and instead optimizing your diet may be the answer.
from Articles https://ift.tt/3zIkSRz
via IFTTT
How Eggs Have Become a Disaster
Omega-3 fats are essential polyunsaturated fatty acids (PUFAs). Your body uses these fats for a variety of functions, such as blood clotting, brain and eye health, digestion and muscle activity.1,2,3
Humans evolved on a diet of omega-6 to omega 3 fats in a ratio of close to 1-to-1.4 However, in the past several decades, the ratio in the stand Western diet measured between 15-to-1 and 16.7-to-1 in 20065 and 10 years later measured at 20-to-1 or greater.6 This shift began during the Industrial Revolution when people began eating foods rich in vegetable oils and cereal grains were fed to livestock, raising the levels of omega-6 fats in meat.7
Omega-3 fats can be broken down into three main categories — alpha linoleic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA).8 ALA is a precursor to EPA and DHA, but it can only be converted in amounts less than 5%.9 DHA and EPA are long-chain omega-3 fats.
You must get each form of omega-3 fat from foods or dietary supplements. ALA is plant-based and found mostly in flaxseed, walnuts, chia seeds and hemp seeds.10 Bioavailable DHA and EPA are found in fish and other marine-based foods.11
There is mounting research that drives home the importance of animal-based omega-3 fats for heart health.12 Deficiency can leave you vulnerable to chronic disease and may increase your risk of poor outcomes in COVID-19.
As I mentioned, the objective is to bring your ratio of omega-6 to omega-3 fatty acids as close to 1-to-1 as possible. Many foods have omega-3 fats, but the ratio of omega-6 to omega 3 is high, so foods other than marine-based fish cannot effectively raise your omega-3 levels.
Omega 3-to-6 Levels in Conventional Eggs Have Plummeted
Farmers used to harvest their eggs from chickens that were free ranging and allowed to forage for their food. For the most part, consumers today have the option of buying four different types of eggs at the grocery store.13,14 They are:
- Conventional — These eggs are produced by cage-raised or cage-free chickens that are grain-fed. Cage-free means the chickens are not in cages, but still are packed into a large room with little space.
- Organic — Hens that produce certified organic eggs receive organic feed and are not treated with hormones. The certification does not necessarily mean they are allowed to forage.
- Pastured or free-range — Hens have some access to the outdoors where they may also have access to their natural food such as plants and insects. The pasture-raised claim15 can be made if there is just a small, bare dirt area, and the free-range claim16 can be made if there is a door that the farm could at some point open. This designation does not indicate what the hens are fed.
- Omega-3 enriched — The hens are raised like conventional chickens and the feed is supplemented with an omega-3 source like flax seeds.
Analysis and comparison of fatty acid composition in conventionally raised and outdoor chickens allowed to forage for insects and plants is vastly different.17 One study published by Cambridge University18 analyzed the difference in the eggs of hens allowed to forage for insects and plants against those fed a commercial diet and kept in cages.
The researchers controlled for the differences in chicken breeds by using sister hens and splitting them into groups. The hens were fed over six weeks before the eggs were analyzed. The researchers split the hens allowed to forage into three groups where one group had access to alfalfa, the second to red-and-white clover and the third to a mix of cool-season grasses.
At the end of the study, they found the concentrations of fatty acids and vitamin A did not differ in the three pastured groups, but those that foraged on grass had 23% more vitamin E then those that foraged on clover.
When they compared the eggs from the caged hens against the pastured eggs they found the hens allowed to forage had “twice as much vitamin E and long-chain omega-3 fats, 2.5-fold more total omega-3 fatty acids, and less than half the ratio of omega-6:omega-3 fatty acids.”19
A later study20 also demonstrated that hens allowed to forage outdoors laid eggs with vitamin D content that was up to four times higher than those who were kept indoors. They compared vitamin D content from the hens exposed to sunlight against free-range eggs purchased at the supermarket and found those from the grocer had relatively low vitamin D content.
Consequences of the Dramatic Shift in Omega Fats
Scientific evidence shows that there have been significant consequences as humans began to eat a diet rich in omega-6 fats and low in omega-3s. The majority of omega-6 fats used to come from nuts and seeds. However current intake comes from processed foods and oxidized vegetable oils.21
This imbalance in omega fats is one route to inflammatory disease, including heart disease, diabetes and cancer. One primary source of omega-6 fats in the American diet is soybean oil, which accounts for 60% of all vegetable oils found in processed foods, salad dressings, snacks and margarine.22
Researchers have linked diets high in soybean oil with Type 2 diabetes and obesity.23 Both of these health conditions are associated with heart disease, impaired cognition, neuropathy and early death.
In recent years it has become increasingly clear that one of the most damaging components in the modern diet is processed vegetable oils, including soybean oil. The biological damage they cause may be even worse than that triggered by refined sugar and high-fructose corn syrup, researchers say.24
The reason is because the oils trigger mitochondrial dysfunction that drives disease processes and several studies25,26,27 have provided scientific evidence of this. The good news is that replacing dangerous oils with healthy saturated fats can go a long way towards boosting your health and reducing your risk of chronic disease.
Unfortunately, many health authority authorities insist that omega-6 rich oils like soybean, corn and canola oil are healthier than saturated animal fats such as pasture-raised butter and lard. This myth has been a tough one to dismantle, despite the evidence against it. To learn more about how processed vegetable oils can harm your health see, “The Case Against Processed Vegetable Oils.”
Many Benefits of Balancing Omega-3 and Omega-6 Ratio
There are significant benefits to balancing your omega-6 and omega-3 ratio. For example, research28 published in 2018 confirmed omega-3 fat can reduce your risk of cardiovascular disease, coronary heart disease and all-cause mortality. Participants with an omega-3 index in the highest quintile had a total mortality 34% lower than those in the lowest quintile, and a 39% lower risk for cardiovascular disease.
As detailed in “More Data Support Heart Healthy Benefits of Omega-3s,” research has found fish oil consumption lowered the risk of all-cause mortality by 13% and cardiovascular mortality by 16%.
DHA is crucial for your brain health. Without enough, your nerve cells become stiff and more prone to inflammation as omega-3 fats are substituted with omega-6. Nerve cells that are rigid and inflamed have lower levels of proper neurotransmission and cells become compromised.29
Low levels of DHA have been linked to memory loss and Alzheimer's disease,30 and some studies suggest degenerative brain diseases may potentially be reversible with sufficient DHA.31,32 Other health benefits include:
|
Reducing inflammation — This can be helpful for those suffering with rheumatoid arthritis by reducing stiffness and pain.33 Women who suffer from menstrual pain may also experience milder symptoms.34,35 |
|
Optimizing muscle building and bone strength — Omega-3 fats help your body build healthy muscle mass, including people suffering from cancer who may experience cachexia.36 Omega-3 fats can also help improve your bone strength by improving the utilization of calcium in your body. This may lead to a reduction in the development of osteoporosis.37,38 |
|
Improving metabolic syndrome39 and insulin resistance.40 |
|
Improving mental health and behavior — Demonstrated benefits have been shown for children with attention deficit hyperactivity disorder (ADHD), including reduced aggression, hyperactivity,41 impulsivity,42 oppositional behavior43 and restlessness.44 Omega-3 is associated with lowered risk for other neurological/cognitive dysfunction as well, including: memory loss, brain aging, learning disorders and ADHD,45 autism and dyslexia.46 |
|
Protecting your vision — DHA is a major structural element in your eye and brain.47 Low levels of DHA may increase your risk for age related macular degeneration.48 |
|
Reducing your risk of kidney disease49 and colon cancer.50 |
Importance of Omega-3 Testing
Like with most other biomarkers, it's impossible to know your omega-3 fatty acid index without testing. The omega-3 index provides the most accurate measurement in the body and should ideally be above 8%.51 The test measures the amount of omega-3 in the red blood cells as a reflection of how much is found in the rest of the body.
Basically, the test measures the average of your intake based on the lifespan of a red blood cell over 120 days. This means it is not influenced by recent meals, but rather an average of the past months. Researchers have used it as an index to analyze data, including that of the Framingham study52 and the Women's Health Initiative.53
Maintaining a level in the range that is associated with low risk can reduce your potential chance of heart disease. An index below 4% has a high risk of heart disease, those with an index from 4% to 8% have an intermediate risk and those with an index greater than 8% have the lowest risk for coronary heart disease.54
Another study55 used randomized control trial results to assess the effects of supplementation on telomere length and oxidative stress. The data suggested that telomere length increases with a decreasing ratio of omega-6 to omega-3. The researchers concluded that even over a short time, a change in the ratio has an impact on cell aging, inflammation and oxidative stress.
Safely Raise Your Omega-3 Intake
If you discover you need more omega-3 after getting tested, consider the different ways you can raise your level without adding toxins. Strategies include reducing or eliminating processed foods as they are high in omega-6 fats and switching to foods that have a lower ratio of omega-6 to omega-3 fats, such as locally raised, outdoor eggs. These are also great sources of omega-3:
• Fish — Small, cold-water fatty fish such as mackerel, anchovies and sardines are excellent sources that have a low risk of hazardous contamination. Wild-caught Alaskan salmon is also low in mercury and other environmental toxins.
Unfortunately, much of the fish supply is heavily polluted with industrial waste, so it is extremely important to be selective, choosing fish high in healthy fats and low in contaminants, such as those mentioned above.
• Krill oil — Krill oil is my preferred choice as a supplement because it has the indispensable animal-based DHA and EPA your body needs, and in a form that's less prone to oxidation.
With the help of phospholipids, the nutrients in krill oil are carried directly to your cell membranes where they are more readily absorbed. Additionally, they may cross your blood-brain barrier to reach important brain structures.
While the following sources may be tempting because they are readily available and cost less than the ones mentioned above, I strongly advise avoiding:
• Farmed salmon — It contains about half the omega-3 levels of wild salmon, is often given antibiotics to treat bacterial infections, and fed a genetically engineered diet of corn and soy products and feed that also may contain or contaminated with pesticides and chicken feathers, poultry litter, genetically modified yeast, chicken fat and dyes.56
• Large carnivorous fish — Marlin, swordfish and tuna (including canned tuna), for example, tend to contain some of the highest concentrations of mercury,57 a known neurotoxin.58
• Fish oil — While fish oil may appear to be a convenient and relatively inexpensive way to increase your intake of omega-3 fats, it typically delivers insufficient antioxidant support. It is also highly prone to oxidation,59 leading to the formation of harmful free radicals.
from Articles https://ift.tt/2TIIWoe
via IFTTT
Media Blasts Oprah for Supporting Alternative Medicine
 In January of this year, Oprah Winfrey invited Suzanne Somers on her show to talk about health tips. The 62-year-old actress uses bio-identical estrogen cream and progesterone on her other arm two weeks a month.
In January of this year, Oprah Winfrey invited Suzanne Somers on her show to talk about health tips. The 62-year-old actress uses bio-identical estrogen cream and progesterone on her other arm two weeks a month.
According to Somers, the bio-identical hormones are identical to the ones created by the human body, unlike conventional hormones, which are made from mare’s urine.
The result has been a media firestorm condemning both Somers and Oprah, including the hit piece in Newsweek linked below. The authors of the piece, Weston Kosova and Pat Wingert, argue that bio-identical hormones are just as synthetic as conventional hormones -- although they don’t much discuss the fact that conventional hormones are actually different from the 17-beta-estradiol made by your body, while the bio-identical hormones are 17-beta-estradiol itself.
The real reason for the attacks on bio-identical hormones?
As Somers points out, many doctors, scientists and media figures make a good deal of money off of the pharmaceutical industry.
And one thing you won’t see mentioned in the Newsweek article is the fact that Pat Wingert is the co-author of a pharmaceutically biased book on hormones and menopause, and that Newsweek is heavily funded by pharmaceutical companies.
This resembles an incident a few years ago when the cattle industry actually sued Oprah Winfrey just for talking about Mad Cow Disease.
from Articles : Hormones, Drugs https://ift.tt/3uExYwy
via IFTTT
How Contraceptive Pill Influences Partner Choice
 The contraceptive pill may disrupt women's natural ability to choose a partner genetically dissimilar to themselves. This could result in difficulties when trying to conceive, an increased risk of miscarriage and long intervals between pregnancies. Passing on a lack of diverse genes to children could also weaken their immune systems.
The contraceptive pill may disrupt women's natural ability to choose a partner genetically dissimilar to themselves. This could result in difficulties when trying to conceive, an increased risk of miscarriage and long intervals between pregnancies. Passing on a lack of diverse genes to children could also weaken their immune systems.Humans tend to be attracted to those with a dissimilar genetic make-up to themselves, maintaining genetic diversity, which is signaled by subtle odors. A research team analyzed how the contraceptive pill affects odor preferences, and found that the preferences of women who began using the contraceptive pill shifted towards men with genetically similar odors.
Not only could genetic similarity in couples lead to fertility problems, but it could ultimately lead to the breakdown of relationships when women stop using the contraceptive pill, as odor perception plays a significant role in maintaining attraction to partners, researchers said.
from Articles : Hormones, Drugs https://ift.tt/3myf0oK
via IFTTT
Do YOU Understand the Dangers of Hormone Therapy?
Despite widespread publicity, the 2002 landmark study on the potential dangers of hormone therapy for postmenopausal women is completely unknown to most women.
New research from the Stanford University School of Medicine discovered that only 29 percent of the women surveyed knew anything about the study two years later. Additionally, only 40 percent of the women were able to identify possible risks and benefits linked to hormone therapy.
Hormone therapy is used to ease your symptoms of menopause, but has also been widely prescribed for preventive purposes, based in part on earlier observational studies that had suggested it could help protect women against heart disease, weak bones, and dementia.
In July 2002, the Women's Health Initiative (WHI) abruptly ended its combination of estrogen and progestin therapy study, as their data discovered higher rates of breast cancer, heart attacks, strokes, and blood clots in the population taking the hormones, compared to those taking placebos.
Later, in April 2004, WHI also halted the portion of the study for estrogen-only therapy, after finding the hormone did not offer any protective heart disease prevention, but rather increased your risk of stroke and blood clots.
The WHI findings triggered enormous changes in the use of hormone therapy, and prescriptions had dropped 38 percent by 2003.
Senior author Randall Stafford, MD, PhD, said their latest survey indicates there's a huge problem in communicating crucial health information to patients effectively, which in turn is indicative of an even larger problem – ensuring that people can make informed decisions about their medical care.
Women's Health Initiative June 21, 2007
WHI March 2, 2007 (The Estrogen-Alone Study Links)
Women's Health Initiative (The Estrogen-Plus-Progestin Study Links)
from Articles : Hormones, Drugs https://ift.tt/38s6otU
via IFTTT
Sally Fitzgibbons on becoming an Olympian at surfing’s inaugural games
from Health | body+soul https://ift.tt/3BOFtWf
Bach’s Rebekah: ‘I cried during my first vinyasa, but it’s taught me so much’
from Health | body+soul https://ift.tt/3iVbO59
‘Slowly but surely meth became my life,’ says Mena Suvari in upcoming memoir
from Health | body+soul https://ift.tt/3l4DTth
Fibromyalgia Linked to Extensive Brain Inflammation
Fibromyalgia, characterized by chronic, widespread pain is an often-debilitating condition that primarily affects women. While as many as 10 million Americans have fibromyalgia, its cause remains a mystery.
Brain scans of fibromyalgia patients have offered hard evidence that the pain they experience is indeed real — mainly because their threshold for tolerating pain impulses is substantially lower than that of most individuals. But the mechanism causing this lowered pain threshold is still unknown.
Some experts, such as Dr. Frederick Wolfe, the director of the National Databank for Rheumatic Diseases and the lead author of the 1990 paper that first defined fibromyalgia's diagnostic guidelines, believe fibromyalgia is mainly a physical response to mental and emotional stress.
But while stress and emotions may indeed play an important role, more recent research shows fibromyalgia patients tend to have severe inflammation in their body, including their nervous system and brain.
Signs and Symptoms of Fibromyalgia
Diagnosis can be a challenge, but the updated case definitions of fibromyalgia, issued in 2010 and later simplified in 2012, claim to correctly diagnose about 83 percent of cases.1 Originally, the condition was thought to be a peripheral musculoskeletal disease. Today, fibromyalgia has become increasingly recognized as a neurobiological problem causing central pain sensitization.
Unfortunately, there are currently no laboratory tests available for diagnosing fibromyalgia, so physicians primarily depend on patient histories, reported symptoms and physical exam findings. Classic symptoms of this condition include:
• Pain — The key marker of fibromyalgia is pain, which is profound, widespread and chronic. Pain inside of your elbows and knees, collarbones and hips is indicative of fibromyalgia when it's present on both sides.
People also frequently report pain all over their bodies — including in their muscles, ligaments and tendons — and the pain tends to vary in intensity. It has been described as deep muscular aching, stabbing, shooting, throbbing and twitching.
Neurological complaints add to the discomfort, such as numbness, tingling and burning. The severity of the pain and stiffness is often worse in the morning. Aggravating factors include cold/humid weather, nonrestorative sleep, fatigue, excessive physical activity, physical inactivity, anxiety and stress.
• Cognitive impairment — So-called "fibro-fog" or foggy-headedness is a common complaint.
• Fatigue — The fatigue of fibromyalgia is different from the fatigue that many people complain of in today's busy world. It is more than being tired; it's an all-encompassing exhaustion that interferes with even the simplest daily activities, often leaving the patient with a limited ability to function both mentally and physically for an extended period of time.
• Sleep disruption — Another major part of the diagnostic criteria for this condition is some type of significant sleep disturbance. In fact, part of an effective treatment program is to make sure you're sleeping better.
Medical researchers have documented specific and distinctive abnormalities in the Stage 4 deep sleep of fibromyalgia patients. During sleep, they are constantly interrupted by bursts of awake-like brain activity, limiting the amount of time they spend in deep sleep.
• Other symptoms — Other common symptoms include irritable bowel and bladder, headaches and migraines, restless leg syndrome and periodic limb movements, impaired memory and concentration, skin sensitivities and rashes, dry eyes and mouth, anxiety, depression, ringing in the ears, dizziness, Raynaud's Syndrome and impaired coordination.
Conventional treatment typically involves some form of pain medication, and perhaps psychotropic drugs like antidepressants. I don't recommend either as they fail to address the cause of your problem. Many fibromyalgia sufferers also do not respond to conventional painkillers, which can set in motion a vicious circle of overmedicating on these dangerous drugs.
Brain Inflammation — Another Hallmark of Fibromyalgia
Using PET imaging, a recent investigation2 by researchers at Massachusetts General Hospital and Karolinska Institutet in Sweden revealed the presence of widespread brain inflammation in patients diagnosed with fibromyalgia.3,4
Earlier research5 conducted at Karolinska Institutet also discovered high concentrations of cytokines (inflammatory proteins) in the cerebrospinal fluid, suggesting fibromyalgia patients have inflammation in their nervous system as well.6
The team at Massachusetts General Hospital, meanwhile, has previously shown that neural inflammation, and glial cell (immune cells) activation specifically, plays a role in chronic back pain. Animal studies have also offered evidence for the hypothesis that glial cell activation can be a cause of chronic pain in general.7
Here, they found that when glial cells in the cerebral cortex were activated, the more aggressive the activation, the greater the fatigue experienced by the patient. As reported by Medical Life Sciences:8
"The current study first assessed fibromyalgia symptoms in patients using a questionnaire. A PET tracer was then used, that is, a radioactive marker which binds a specific protein called translocator protein (TSPO) that is expressed at levels much above the normal in activated glial cells, namely, astrocytes and microglia …
[G]lial activation was found to be present at significantly higher levels in multiple brain areas in patients who had fibromyalgia than in controls. Glial cell activation causes inflammatory chemicals to be released, which cause the pain pathways to be more sensitive to pain, and promote fatigue …
One area showing higher TSPO binding in direct proportion to the self-reported level of fatigue was the cingulate gyrus, an area of the brain linked to emotional processing. Previous research has reported that this area is inflamed in chronic fatigue syndrome."
Brain Inflammation Linked to Loss of Brain Cells
In related news, German researchers investigating inflammation mechanisms in the brain have found that as mice get older and regulation of inflammatory responses become increasingly impaired, they start losing brain cells.9
Interestingly, the cannabinoid receptor type 1 (CB1), which produces the "high" in response to tetrahydrocannabinol (THC) in marijuana, also helps regulate inflammatory reactions in your brain. In short, chronic brain inflammation is in part driven by the CB1 receptors' failure to respond. To understand how this works, you need to know a little bit about how microglial cells work.
Microglial cells are specialized immune cells found in your central nervous system, including your spinal cord and brain. These immune cells respond to bacteria and are responsible for clearing out malfunctioning nerve cells. They also signal and recruit other immune cells when needed and trigger the inflammatory response when necessary.
Problems arise when the inflammatory response becomes dysregulated and overactive. In the brain, the inflammation can easily damage healthy brain tissue. The "brake signal" that instructs glial cells to stop their inflammatory activity is endocannabinoids, and the endocannabinoids work by binding to certain receptors, including CB1 and cannabinoid receptor type 2 (CB2).
Immune Cells Communicate and Influence Inflammatory Response Using Endocannabinoids
Curiously, microglial cells have virtually no CB1 and very few CB2 receptors, yet they still react to endocannabinoids. The present study was designed to investigate this puzzling riddle. As it turns out, there's a type of neuron that does contain a large number of CB1 receptors, and it appears that it is the CB1 receptors on these specific neurons that control microglial cell activity.
In other words, it appears microglial cells do not communicate with nerve cells directly; rather, they release endocannabinoids, which then bind to CB1 receptors found in nearby neurons. These neurons in turn communicate directly with other nerve cells. So, the brain's immune response is regulated in an indirect manner rather than a direct one.
Now, what happens with age is that your natural production of endocannabinoids decreases, which then leads to impaired immune response regulation and chronic inflammation. As noted by coauthor Dr. Andras Bilkei-Gorzo:10
"Since the neuronal CB1 receptors are no longer sufficiently activated, the glial cells are almost constantly in inflammatory mode. More regulatory neurons die as a result, so the immune response is less regulated and may become free-running."
Earlier research11 by this same team found that THC can help restore cognitive function in older brains, and the current study also hints at THC-containing cannabis may have valuable neuroprotective benefits in older people by quelling brain inflammation and preventing loss of brain cells. As the study was done on mice, further research is needed to confirm that the same mechanisms apply to humans, but it's compelling nonetheless.
Are You Living an Inflammatory Lifestyle?
Your diet can either promote or decrease inflammation. For example, foods that increase the inflammatory response in your body include:
- Sugar, especially processed corn syrup
- Synthetically produced trans fats
- Processed vegetable and seed oils, high in oxidized omega-6 fat
- Processed meats
- Refined carbohydrates
Meanwhile, marine-based omega-3 fats have powerful anti-inflammatory effects, and are crucial for healthy brain function in general. Antioxidant-rich fruits and vegetables are also important for controlling inflammation, as is optimizing your vitamin D to a level of 60 to 80 ng/mL, ideally through sensible sun exposure.
In addition to anti-inflammatory and immune-boosting properties, vitamin D receptors appear in a wide variety of brain tissue, and researchers believe optimal vitamin D levels may enhance important chemicals in your brain and protect brain cells by increasing the effectiveness of glial cells that help nurse damaged neurons back to health.
A number of ubiquitous chemicals have also been implicated in inflammation, so if you struggle with fibromyalgia you'd be wise to take a close look at your choice of foods, household and personal care products. As mentioned earlier, getting enough high-quality sleep is another key treatment component for fibromyalgia.
Ketogenic Diet Massively Decreases Brain Inflammation
Research12 published last year suggests ketogenic diets — which are high in healthy fats and low in net carbs — are a particularly powerful ally for suppressing brain inflammation, as ketones are powerful HDAC (histone deacetylase inhibitors) that suppress the primary NF-κB inflammatory pathway.
As explained by Medical Xpress,13 the defining moment of the study14 came when the team "identified a pivotal protein that links the diet to inflammatory genes, which, if blocked, could mirror the anti-inflammatory effects of ketogenic diets."
A ketogenic diet changes the way your body uses energy, converting your body from burning carbohydrates for energy to burning fat as your primary source of fuel. When your body is able to burn fat, your liver creates ketones, which burn more efficiently than carbs, thus creating far less reactive oxygen species and secondary free radicals that can damage your cellular and mitochondrial cell membranes, proteins and DNA.
Animals (rats) used in this study were found to have reduced inflammation when the researchers used a molecule called 2-deoxyglucose (2DG) to block glucose metabolism and induce a ketogenic state, similar to what would occur if you followed a ketogenic diet. By doing this, inflammation was brought down to levels near those found in controls.
Suppressing Inflammation Improves Pain
Senior study author Dr. Raymond Swanson, a professor of neurology at UCSF and chief of the neurology service at the San Francisco Veterans Affairs Medical Center, commented on the results, saying:
"I was most surprised by the magnitude of this effect, because I thought ketogenic diets might help just a little bit. But when we got these big effects with 2DG, I thought wow, there's really something here.
The team further found that reduced glucose metabolism lowered a key barometer of energy metabolism — the NADH/NAD+ ratio — which in turn activated a protein called CtBP that acts to suppress activity of inflammatory genes."
The study also pointed out that a ketogenic diet may relieve pain via several mechanisms, similar to the ways it's known to help epilepsy.
"Like seizures, chronic pain is thought to involve increased excitability of neurons; for pain, this can involve peripheral and/or central neurons. Thus, there is some similarity of the underlying biology," the authors stated, adding:
"A major research focus should be on how metabolic interventions such as a ketogenic diet can ameliorate common, comorbid and difficult-to-treat conditions such as pain and inflammation."15
Cyclical Ketosis for Optimal Health
Eating a ketogenic diet doesn't have to be complicated or painful. My book "Fat for Fuel" presents a complete Mitochondrial Metabolic Therapy (MMT) program, complemented by an online course created in collaboration with nutritionist Miriam Kalamian, who specializes in nutritional ketosis.
The course, which consists of seven comprehensive lessons, teaches you the keys to fighting chronic disease and optimizing your health and longevity. In summary, the MMT diet is a cyclical ketogenic diet, high in healthy fats and fiber, low in net carbs with a moderate amount of protein.
The cyclical component is important, as long-term continuous ketosis has drawbacks that may actually undermine your health and longevity. One of the primary reasons to cycle in and out of ketosis is because the "metabolic magic" in the mitochondria actually occurs during the refeeding phase, not during the starvation phase.
Ideally, once you have established ketosis you cycle healthy carbs back in to about 100 to 150 grams on days when you do strength training. MMT has a number of really important health benefits, and may just be the U-turn you've been searching for if you're struggling with a chronic health condition. You can learn more by following the hyperlinks provided in the text above.
Address Emotional Contributors
Since fibromyalgia is a chronic condition, it becomes emotionally challenging in addition to the physical challenges it imposes on your life. Having a game plan to deal with your emotional well-being is especially important if you suffer from any chronic disease.
If you have fibromyalgia, you might be able to trace it back to a triggering event, or you might not. Any traumatic experience has the potential to linger in your mind for a lifetime. You can have the perfect diet, the perfect exercise routine, and an ideal life; but if you have lingering unresolved emotional issues, you can still become very sick.
A tool that can help release this emotional sludge is the Emotional Freedom Techniques (EFT). If you are a regular reader of my newsletter, this won't be an unfamiliar term to you. EFT is a form of bioenergetic normalization. If you have fibromyalgia, this is something that is going to be extremely helpful. You can do this yourself, at home, and it takes just a few minutes to learn. For a demonstration, see the video above.
from Articles : Fibromyalgia https://ift.tt/2RY3F1l
via IFTTT
Foods That Chronic Pain Sufferers Need to Avoid
 Chronic pain is a pervasive issue and fibromyalgia is a very common form. It is a chronic condition whose symptoms include muscle and tissue pain, fatigue, depression, and sleep disturbances.
Chronic pain is a pervasive issue and fibromyalgia is a very common form. It is a chronic condition whose symptoms include muscle and tissue pain, fatigue, depression, and sleep disturbances.
Recent data suggests that central sensitization, in which neurons in your spinal cord become sensitized by inflammation or cell damage, may be involved in the way fibromyalgia sufferers process pain.
Certain chemicals in the foods you eat may trigger the release of neurotransmitters that heighten this sensitivity.
Although there have been only a handful of studies on diet and fibromyalgia, the following eating rules can’t hurt, and may help, when dealing with chronic pain.
Limit Sugar as Much as Possible. Increased insulin levels will typically dramatically worsen pain. So you will want to limit all sugars and this would typically include fresh fruit juices. Whole fresh fruit is the preferred method for consuming fruit products.
If you are overweight, have high blood pressure, high cholesterol or diabetes, you will also want to limit grains as much as possible as they are metabolized very similarly to sugars. This would also include organic unprocessed grains. Wheat and gluten grains are the top ones to avoid.
Eat fresh foods. Eating a diet of fresh foods, devoid of preservatives and additives, may ease symptoms triggered by coexisting conditions such as irritable bowel syndrome (IBS).
It’s also a good idea to buy organic food when possible, as it’s best to avoid pesticides and chemicals. However, fresh is best. So if you have to choose between local, fresh, non-organic and organic but wilting – go with fresh, and clean properly.
Avoid caffeine. Fibromyalgia is believed to be linked to an imbalance of brain chemicals that control mood, and it is often linked with inadequate sleep and fatigue. The temptation is to artificially and temporarily eliminate feelings of fatigue with stimulants like caffeine, but this approach does more harm than good in the long run. Though caffeine provides an initial boost of energy, it is no substitute for sleep, and is likely to keep you awake.
Try avoiding nightshade vegetables. Nightshade vegetables like tomatoes, potatoes, and eggplant may trigger arthritis and pain conditions in some people.
Be Careful with Your Fats. Animal based omega-3 fats like DHA and EPA have been touted as a heart-healthy food, and they may help with pain, as well. They can help reduce inflammation and improve brain function. At the same time, you want to eliminate all trans fat and fried foods, as these will promote inflammation.
Use yeast sparingly. Consuming yeast may also contribute to the growth of yeast fungus, which can contribute to pain.
Avoid pasteurized dairy. Many fibromyalgia sufferers have trouble digesting milk and dairy products. However, many find that raw dairy products, especially from grass fed organic sources, are well tolerated.
Cut down on carbs. About 90 percent of fibromyalgia patients have low adrenal functioning, which affects metabolism of carbohydrates and may lead to hypoglycemia.
Avoid aspartame. The artificial sweetener found in some diet sodas and many sugar-free sweets is part of a chemical group called excitotoxins, which activate neurons that can increase your sensitivity to pain.
Avoid additives. Food additives such as monosodium glutamate (MSG) often cause trouble for pain patients. MSG is an excitatory neurotransmitter that may stimulate pain receptors; glutamate levels in spinal fluid have been shown to correlate with pain levels in fibromyalgia patients.
Stay away from junk food. Limit or eliminate fast food, candy, and vending-machine products. In addition to contributing to weight gain and the development of unhealthy eating habits, these diet-wreckers may also irritate your muscles, disrupt your sleep, and compromise your immune system.
from Articles : Fibromyalgia https://ift.tt/1wN9XCc
via IFTTT
How to Avoid Being Fooled at the Supermarket
from Articles : Fibromyalgia https://ift.tt/3v79wVQ
via IFTTT
Proof That Fibromyalgia is Real
 Researchers have detected abnormalities in the brains of people with fibromyalgia, a chronic condition whose symptoms include muscle pain and fatigue.
Researchers have detected abnormalities in the brains of people with fibromyalgia, a chronic condition whose symptoms include muscle pain and fatigue.Some researchers have suggested that the pain of fibromyalgia is the result of depression, but the new study suggests otherwise. The abnormalities were independent of anxiety and depression levels.
Researchers evaluated 20 women diagnosed with fibromyalgia and 10 healthy women without the condition who served as a control group. The researchers performed brain imaging called single photon emission computed tomography, or SPECT.
The imaging showed that women with the syndrome had "brain perfusion" -- blood flow abnormalities in their brains. The abnormalities were directly correlated with the severity of disease symptoms.
An increase in blood flow was found in the brain region known to discriminate pain intensity.
from Articles : Fibromyalgia https://ift.tt/3vbtoqH
via IFTTT
Are You Allergic to Wireless Internet?
 Electromagnetic Hypersensitivity Syndrome (EHS) is a condition in which people are highly sensitive to electromagnetic fields. In an area such as a wireless hotspot, they experience pain or other symptoms.
Electromagnetic Hypersensitivity Syndrome (EHS) is a condition in which people are highly sensitive to electromagnetic fields. In an area such as a wireless hotspot, they experience pain or other symptoms.
People with EHS experience a variety of symptoms including headache, fatigue, nausea, burning and itchy skin, and muscle aches. These symptoms are subjective and vary between individuals, which makes the condition difficult to study, and has left experts divided about the validity of such claims.
More than 30 studies have been conducted to determine what link the condition has to exposure to electromagnetic fields from sources such as radar dishes, mobile phone signals and, Wi-Fi hotspots.
from Articles : Fibromyalgia https://ift.tt/1bYDXku
via IFTTT
Measuring creativity, one word at a time
from Top Health News -- ScienceDaily https://ift.tt/3BKeJ9j
Olympian Jess Fox on what Tokyo is really like
from Health | body+soul https://ift.tt/373WaPq
Delta Variant: Natural Immunity 700% Better Than the Vaccine
A recurring theme being broadcast by public health officials and the media is that vaccine-induced immunity is superior to that of natural immunity, but preliminary data from Israel — a country with more than 60% of its population vaccinated against COVID-191 — is showing otherwise.
Data presented to the Israeli Health Ministry July 13, 2021,2 revealed that, of the more than 7,700 COVID-19 cases reported since May 2021, only 72 occurred in people who had previously had COVID-19 — a rate of less than 1%. In contrast, more than 3,000 cases — or approximately 40% — occurred in people who had received a COVID-19 vaccine. As reported by Israeli National News:
“With a total of 835,792 Israelis known to have recovered from the virus, the 72 instances of reinfection amount to 0.0086% of people who were already infected with COVID.
By contrast, Israelis who were vaccinated were 6.72 times more likely to get infected after the shot than after natural infection, with over 3,000 of the 5,193,499, or 0.0578%, of Israelis who were vaccinated getting infected in the latest wave.”
In other words, those who were vaccinated were nearly 700% more likely to develop COVID-19 than those who had natural immunity from a prior infection — and this is largely in response to the Delta variant, which has led to increasing infections in Israel.3
Rate of COVID Reinfection: 0.27%
It’s extremely rare to get reinfected by COVID-19 after you’ve already had the disease and recovered. How rare? Researchers from Ireland conducted a systematic review including 615,777 people who had recovered from COVID-19, with a maximum duration of follow-up of more than 10 months.4
“Reinfection was an uncommon event,” they noted, “… with no study reporting an increase in the risk of reinfection over time.” The absolute reinfection rate ranged from 0% to 1.1%, while the median reinfection rate was just 0.27%.5,6,7
Another study revealed similarly reassuring results. It followed 43,044 SARS-CoV-2 antibody-positive people for up to 35 weeks, and only 0.7% were reinfected. When genome sequencing was applied to estimate population-level risk of reinfection, the risk was estimated at 0.1%.8
Again, there was no indication of waning immunity over seven months of follow-up, with the researchers concluding, “Reinfection is rare. Natural infection appears to elicit strong protection against reinfection with an efficacy >90% for at least seven months.”9
Another study from Israel also had researchers questioning “the need to vaccinate previously-infected individuals,” after their analysis showed similar risks of reinfection among those with vaccine-induced or natural immunity. Specifically, vaccination had an overall estimated efficacy of preventing reinfection of 92.8%, compared to 94.8% for natural immunity acquired via prior infection.10
Why Natural Immunity Is Superior
Speaking with journalist Daniel Horowitz, pathologist Dr. Ryan Cole explained that natural immunity produces broad immunity that can’t be matched by vaccination:11
"A natural infection induces hundreds upon hundreds of antibodies against all proteins of the virus, including the envelope, the membrane, the nucleocapsid, and the spike. Dozens upon dozens of these antibodies neutralize the virus when encountered again.
Additionally, because of the immune system exposure to these numerous proteins (epitomes), our T cells mount a robust memory, as well. Our T cells are the 'marines' of the immune system and the first line of defense against pathogens. T cell memory to those infected with SARSCOV1 is at 17 years and running still."
In 2020 it was reported that people who had recovered from SARS-CoV — a virus that is genetically closely related to SARS-CoV-2 and belongs to the same viral species — maintained significant levels of neutralizing antibodies at least 17 years after initial infection.12 This also suggests that long-term natural immunity against SARS-CoV-2 should be expected.13
With vaccination, however, Israeli14 data suggest that those who were vaccinated early on, in January 2021, are becoming susceptible to the virus, suggesting its efficacy may wane after about six months.
This sentiment was echoed by Pfizer’s head of medical research and development, Mikael Dolsten, who said “after six months, there may be risk of infection with the expected decline of antibodies.” Pfizer is seeking emergency use authorization for a third booster dose of its COVID-19 vaccine in the U.S.15
According to Cole, part of the reason for waning vaccine-induced immunity is because “we mount an antibody response to only the spike and its constituent proteins” and “as the virus preferentially mutates at the spike, these proteins are shaped differently and antibodies can no longer ‘lock and key’ bind to these new shapes.”16
Natural COVID Immunity May Last a Lifetime
It was initially suggested that natural COVID-19 immunity may be short-lived. This was based on early data on SARS-CoV-2, which found that antibody titers declined rapidly in the first months after recovery from COVID-19. According to a team of researchers from the Washington University School of Medicine, however, if you’ve had COVID-19 — even a mild case — you’re likely to be immune for life, as is the case with recovery from many infectious agents.17
According to senior author of the study Ali Ellebedy, Ph.D., an associate professor of pathology and immunology at Washington University School of Medicine in St. Louis, “It’s normal for antibody levels to go down after acute infection, but they don’t go down to zero; they plateau.”18
The researchers found a biphasic pattern of antibody concentrations against SARS-CoV-2, in which high antibody concentrations were found in the acute immune response that occurred at the time of initial infection. The antibodies declined in the first months after infection, as should be expected, then leveled off to about 10% to 20% of the maximum concentration detected.
When a new infection occurs, cells called plasmablasts provide antibodies, but when the virus is cleared, longer lasting memory B cells move in to monitor blood for signs of reinfection.19 Bone marrow plasma cells (BMPCs) also exist in bones, acting as “persistent and essential sources of protective antibodies.”20 Ellebedy even said the protection provided by naturally acquired immunity is likely to continue “indefinitely”:21
“These [BMPC] cells are not dividing. They are quiescent, just sitting in the bone marrow and secreting antibodies. They have been doing that ever since the infection resolved, and they will continue doing that indefinitely.”
In another explanation of why antibody levels drop after initial infection — but it’s not an indication of waning immunity — Cole told Horowitz:22
“Yes, our antibody levels drop over time, however, scientifically, the memory B cells that make antibodies have been proven to be present in our lymph nodes and bone marrow. They are primed and ready to produce a broad array of antibodies upon viral pre-exposure.
It would be physiologically, energetically impossible to maintain high antibody levels to all the pathogens we are constantly exposed to, and we would look like the ‘swollen Stay-Puft marshmallow man’ of lymph nodes, constantly, if the immune system were required to do that.”
Why Are Natural Immunity, Early Treatment Protocols Censored?
Dr. Peter McCullough is an internist, cardiologist, epidemiologist and full professor of medicine at Texas A&M College of Medicine in Dallas. He also has a master's degree in public health and is known for being one of the top five most-published medical researchers in the U.S. and is the editor of two medical journals.
In our recent interview, he discussed the importance of early treatment for COVID-19, and the potential motivations behind the suppression of safe and effective treatments. He also told Horowitz, “[T]here has never been a confirmed second [COVID-19] infection beyond 90 days with similar or worse cardinal symptoms and confirmed PCR/Antigen/Sequencing test."23
In August 2020, McCullough's landmark paper "Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 Infection" was published online in the American Journal of Medicine.24 The follow-up paper, titled "Multifaceted Highly Targeted Sequential Multidrug Treatment of Early Ambulatory High-Risk SARS-CoV-2 Infection (COVID-19)," was published in Reviews in Cardiovascular Medicine in December 2020.25
While early treatment options were available when the pandemic began, patients were simply told to stay home and do nothing, until the infection had progressed to the point where they were having trouble breathing. Once at the hospital, COVID patients were routinely placed on mechanical ventilation — a practice that was quickly discovered to be lethal.
But McCullough has been an outspoken advocate for early treatment for COVID, as have other pioneering doctors like those behind the MATH+ protocol. He believes the end goal in suppressing early treatment was to secure the rollout of a mass vaccination campaign.
Indeed, effective treatments like ivermectin — a broad-spectrum antiparasitic that also has anti-inflammatory activity — have shown remarkable success in preventing and treating COVID-19,26 but they continue to be ignored in favor of more expensive, and less effective, treatments and mass experimental vaccination.27
At this point, however, with effective treatments available, the documented high survival rate of COVID-1928 and knowledge that if you’ve had COVID-19, you’re already likely immune to further infection, the rationale for getting vaccinated is faltering. Even the Delta variant has a very low 0.2% case fatality rate in the U.K., which drops to 0.03% in those under 50.29
Natural Infection Will ‘Burn Out All Variants’
If you choose to get a COVID-19 vaccine, you’re participating in an unprecedented experiment with an unapproved gene therapy, of which the benefits may not outweigh the risks, especially if you’ve already had COVID-19 and are already likely immune.
As noted by Horowitz, “Natural infection is the only phenomena that will ultimately burn out all variants, and the entire focus should be on getting seniors and other vulnerable people early treatment the minute they feel symptoms and even a prophylactic regimen of ivermectin … when appropriate.”30
Meanwhile, McCullough pointed out that by getting vaccinated, you’re setting yourself up for a very narrow immunity — much unlike the broad naturally acquired immunity — that could be easily overwhelmed by a more virulent virus. As he said in our interview that I previously mentioned:
“What I know based on the literature right now is there could be a risk given the narrow spectrum of immunologic coverage … There could be such a narrow immunity that more virulent strain could overwhelm it …
The most recent variant is the Delta variant. That's the weakest of all the variants and the most easily treatable. But if someone, let's say a nefarious entity created a more virulent virus, it could easily be designed to scoot past a very narrow immunity that hundreds of millions, if not billions of people, will be keyed to with narrow immunity."
from Articles https://ift.tt/3BKoDIg
via IFTTT
Signs of COVID Injection Failure Mount
In recent weeks, a number of signs have emerged indicating the COVID-19 injections cannot put an end to COVID-19 outbreaks. In the July 15, 2021, video report above, Dr. John Campbell reviews data coming out of the U.K. On a side note, I do not agree with everything Campbell says in this video, such as promoting mask wearing, for example. It’s his data review that is of interest here.
As noted in the video, as of July 15, 87.5% of the adult population in the U.K. had received one dose of COVID-19 “vaccine” and 67.1% had received two. Yet symptomatic cases among partially and fully “vaccinated” are now suddenly on the rise, with an average of 15,537 new infections a day being detected, a 40% increase from the week before.
Meanwhile, the daily average of new symptomatic cases among unvaccinated is 17,588, down 22% from the week before. This suggests the wave among unvaccinated has peaked and that natural herd immunity has set in, while “vaccinated” individuals are becoming more prone to infection.
U.K. hospitals are confirming double-injected patients are part of the patient population being treated for active COVID infection, and two cities have issued public warnings to their residents, letting them know they may end up in the hospital even if they’ve been double-injected against COVID-19.
“There are currently 15 patients in hospital with COVID across the Trust; last month there were none,” The Yorkshire Post reported1 July 9, 2021. An undisclosed number of them had received two doses of COVID “vaccine.”
“The message I would like to share with you all is that some of their patients are double vaccinated,” Heather McNair, chief nurse at York and Scarborough Teaching Hospitals, told the Post.2
“This is a disease that can still affect you and still make you poorly when you are double vaccinated. We have got a ward at the moment full of COVID patients in our hospital and that is not going away anytime soon.”
While the number of hospitalized COVID patients doubled in a single week, the total number was still well below the number reported in January 2021 — a statistic Amanda Bloor, accountable officer for the NHS North Yorkshire Clinical Commissioning Group, takes as proof that the injection program is “having the anticipated impact around reducing the risk of death and reducing serious illness.”
COVID Surges in Countries with Highest Injection Rates
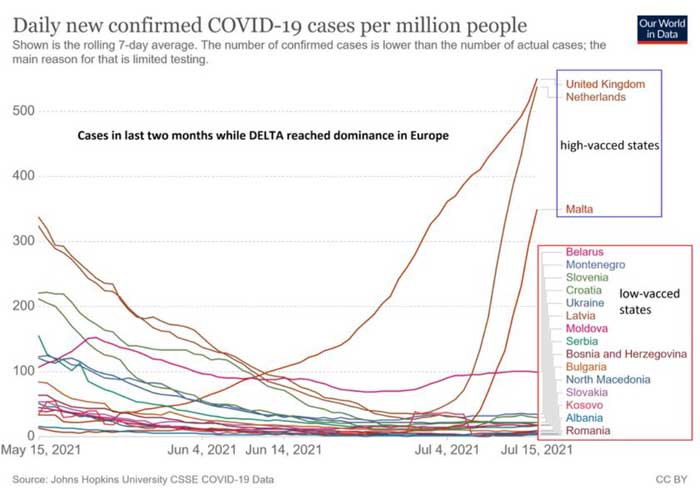
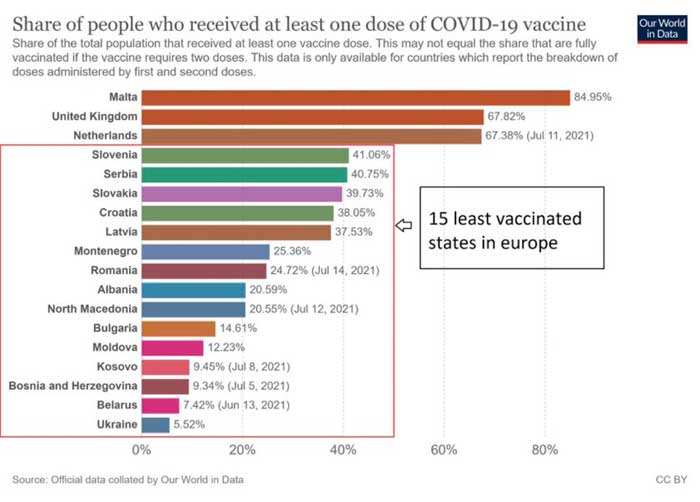
I wouldn’t be so quick to assume lower hospitalization rates in the middle of summer are a sign that the injections are having a positive impact. We also have data3 showing that countries with the highest COVID injection rates are also experiencing the greatest upsurges in cases, while countries with the lowest injection rates have the lowest caseloads. This trend “is worrying me quite a bit,” Dr. Robert Malone, inventor of the mRNA vaccine technology, said in a July 16, 2021, Tweet.4
You can view more data in this thread, posted by Corona Realism.5 Cyprus, where more than 51% of residents have received the jab, now has the highest case count in the world. Interestingly, the outbreak on the British Navy ships — which I’ll cover further below — occurred shortly after a stopover in Cyprus.6
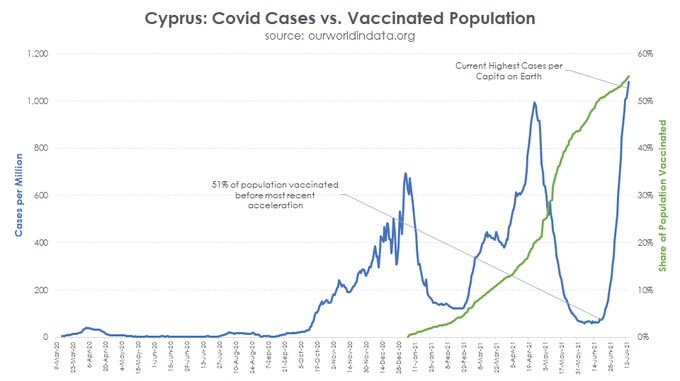
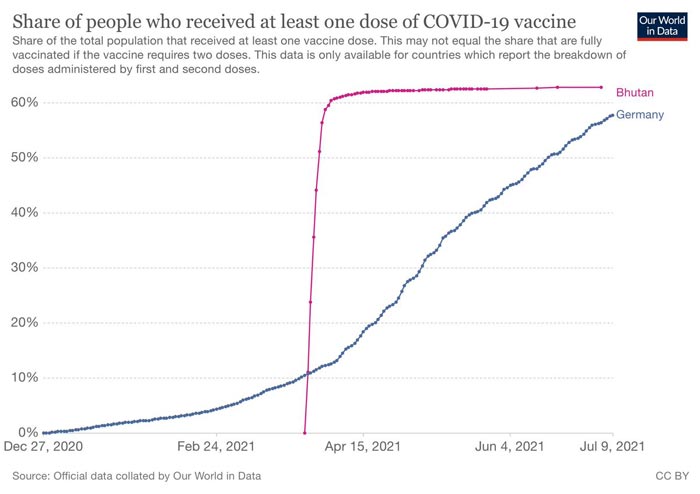
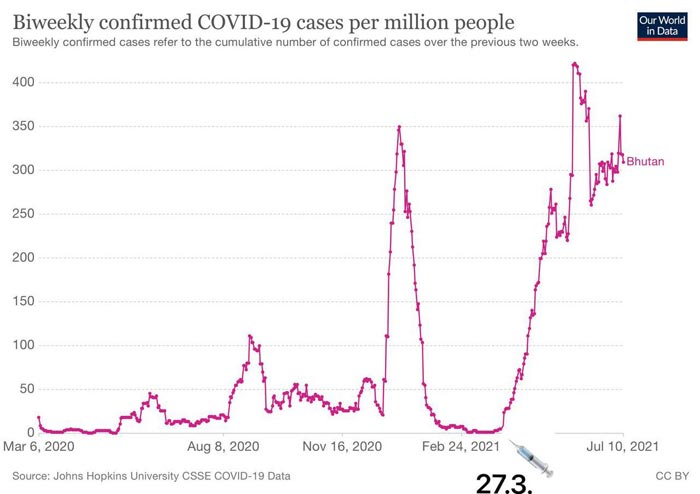
Bhutan offers an interesting glimpse into the effects of mass COVID “vaccination”. They managed to get 64% of residents injected in just one week, starting March 27, 2021, and almost immediately, there was a rapid uptick in cases.
In the first graph below, you see the extraordinarily rapid injection rate in Bhutan, going from zero to 64% in a matter of days. In the second graph, you can see the effect on cases in the weeks that followed. They went from near-zero cases at the outset of the injection campaign, to a high of more than 400 cases per million in the weeks following.
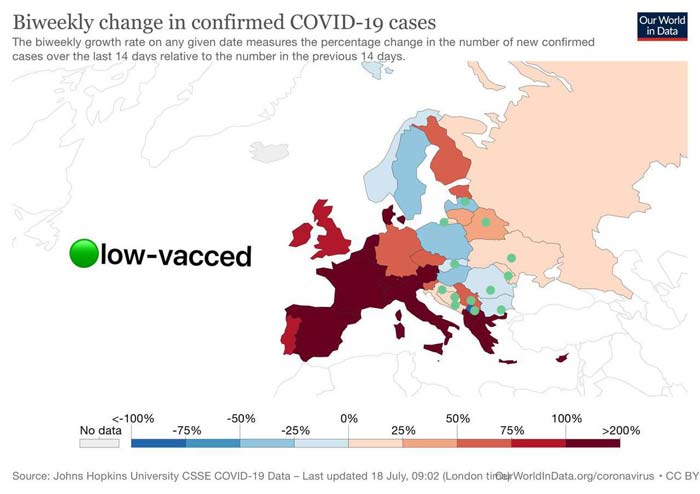
Case Counts Lowest in Low-‘Vaxxed’ Nations
On the flipside, we see the lowest number of positive COVID tests congregated in nations that also have the lowest rates of COVID “vaccine” uptake. While it’s not a 100% clear-cut correlation, it is a trend, and we also have to remember that the PCR tests have issues that complicate any attempt at data analysis.
The main problem is that if you run the PCR test at too-high a cycle threshold (CT), you end up with an inordinate number of false positives.7,8,9 The CT refers to the point in the test where a positive result is obtained. A CT of 35 or higher will give you a 97% false positive rate.10
For maximum accuracy, you’d have to use a CT of 17.11 It’s unclear what all these countries are using, but it’s unlikely they’re using a CT below 20 as a matter of routine. This means most case counts around the world will be falsely elevated.
This is particularly true for unvaccinated individuals in the U.S., as their tests are recommended to be run at a CT of 40, whereas patients that have received a COVID injection will have their COVID tests run at a CT below 28. This makes it appear as though the case rate is higher among the unvaccinated, when in reality it’s just an artifact from highly biased testing and few of these falsely positive “cases” are actually sick.
Looking at the hospitalization rate for confirmed COVID-19 in the U.S.,12 we see that the number of people sick enough to require medical attention is nowhere near what it was during the winter months of 2021, and since only 5.9% of American adults had been injected with two doses as of February 21, 2021,13 we can conclude that the injections did not cause this rapid decline in hospitalizations.
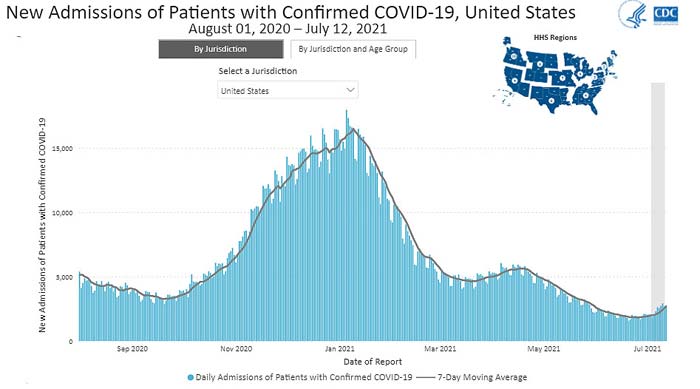
The best explanation for the decline in both cases and hospitalizations after the rollout of COVID shots is the emergence of natural herd immunity from previous infections.
In a July 12, 2021, STAT News article,14 Robert M. Kaplan, Professor Emeritus at the UCLA Fielding School of Public Health, calculated that by April 2021, the natural immunity rate was above 55% in 10 U.S. states, and in most of those same states, new infections were in rapid decline as early as the end of 2020, at a time when only a tiny fraction of the population had received their shots.
CDC Doesn’t Track All Breakthrough Cases
We must also remember that the U.S. Centers for Disease Control and Prevention are artificially driving down case rates, hospitalization rates and death rates for “vaccinated” Americans by selectively tracking breakthrough cases. They only track and report breakthrough cases where the patient is hospitalized or dies.15 They do not count mild cases, even if they have a positive test result.
A number of media outlets have expressed concerns about this biased tracking and reporting. As noted in Harvard Health,16 the CDC’s strategy prevents us from ascertaining whether one injection is more or less effective than another. It can also hide manufacturing problems and prevent us from determining whether timing of the second dose might have a bearing on effectiveness, as well as a number of other things.
Business Insider17 pointed out that not tracking all breakthrough cases makes it more difficult to determine how dangerous the Delta variant really is. NPR expresses a similar view, stating that “Critics argue the strategy could miss important information that could leave the U.S. vulnerable, including early signs of new variants that are better at outsmarting the vaccines.”18
Even Complete ‘Vaccine’ Coverage Won’t Stop Infections
July 14, 2021, BBC News reported19 100 fully injected crewmembers had tested positive onboard the British Defense aircraft carrier HMS Queen Elizabeth. It’s unclear whether any of them actually have symptoms. According to British defense secretary Ben Wallace, mitigation efforts include mask wearing, social distancing and a track and trace system. He made no mention of actual treatment for acute infection.
Other warships are also reporting onboard outbreaks, although Wallace did not offer any details about them. The fleet is currently in the Indian Ocean and plans to continue the 28-week deployment, with Japan as their destination. BBC News said the queen and prime minister had been onboard the flagship shortly before it sailed.
This case offers a sobering view into the effectiveness of these gene modifying shots, as the HMS Queen Elizabeth now has a case rate of 1 in 1620 — the highest case rate recorded so far, that I know of. Yet 100% of the crew has been double-injected. This tells you that the vaccine-induced herd immunity narrative is a fairytale. These injections apparently cannot prevent COVID-19 even if 100% of a given population gets them!
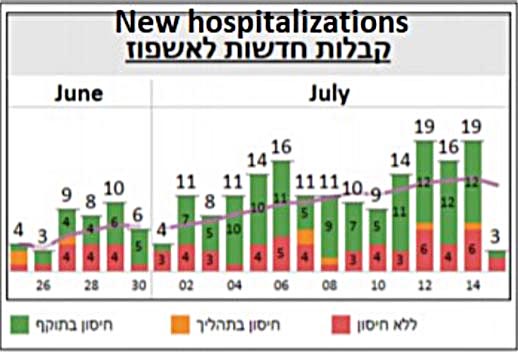
Israeli Data Indicate Pfizer ‘Vaccine’ Failure
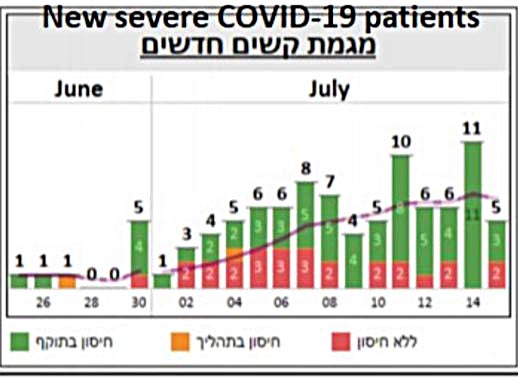
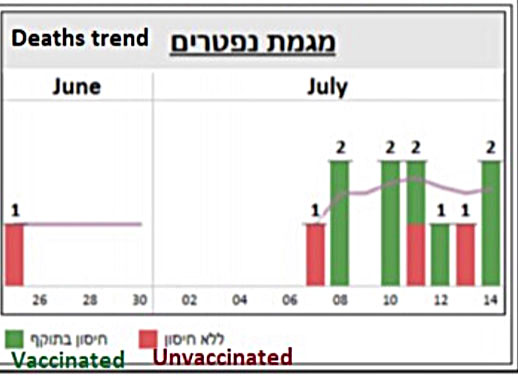
Data from Israel also offer a dismal view of COVID-19 injections. Israel used Pfizer’s mRNA injection exclusively, so this gives us a good idea of its effectiveness. Overall, it looks like an abysmal failure, as a majority of serious cases and deaths are now occurring among those injected with two doses. The following is a screenshot of graphs posted on Twitter.21
The red is unvaccinated, yellow refers to partially “vaccinated” and green fully “vaccinated” with two doses. The charts speak for themselves.
Overall, it doesn’t appear as though COVID-19 gene modification injections have the ability to effectively eliminate COVID-19 outbreaks, and this makes sense, seeing how it’s mathematically impossible for them to do so.
The four available COVID shots in the U.S. provide an absolute risk reduction between just 0.7% and 1.3%.22,23 (Efficacy rates of 67% to 95% all refer to the relative risk reduction.) Meanwhile, the noninstitutionalized infection fatality ratio across age groups is a mere 0.26%.24 Since the absolute risk that needs to be overcome is lower than the absolute risk reduction these injections can provide, mass vaccination simply cannot have a favorable impact.
CDC Tries to Hide COVID Jab Death Toll
They can, however, cause unnecessary deaths among otherwise healthy individuals. Tragically, the CDC is doing everything it can to hide just how great that death toll is. In what appears to be a deliberate attempt at deception, the CDC “rolled back” its July 19, 2021, adverse events report to statistics from the previous week. I’ll explain. Take note of the specific dates and death totals in each of the following excerpts. The July 13 report reads as follows:25
“Reports of death after COVID-19 vaccination are rare. More than 334 million doses of COVID-19 vaccines were administered in the United States from December 14, 2020, through July 12, 2021. During this time, VAERS received 6,079 reports of death (0.0018%) among people who received a COVID-19 vaccine.”
The original July 19 report (saved on Wayback) initially read as follows:26
“Reports of death after COVID-19 vaccination are rare. More than 338 million doses of COVID-19 vaccines were administered in the United States from December 14, 2020, through July 19, 2021. During this time, VAERS received 12,313 reports of death (0.0036%) among people who received a COVID-19 vaccine.”
Please note, the death toll more than doubled in a single week. That original July 19 report was then changed to this. The date on the report is still July 19:27
“Reports of death after COVID-19 vaccination are rare. More than 334 million doses of COVID-19 vaccines were administered in the United States from December 14, 2020, through July 13, 2021. During this time, VAERS received 6,079 reports of death (0.0018%) among people who received a COVID-19 vaccine.”
At a time when accuracy and transparency is of such critical importance for informed consent, it’s beyond shocking to see the CDC engage in this kind of deception. Yet here we are. We’re now living in a world where crucial public health data is being manipulated at every turn. For this reason, looking at larger trends such as those reviewed above may offer a more dependable picture of what the real-world consequences of these shots are.
from Articles https://ift.tt/3i62dcm
via IFTTT