The Role of Magnesium for Cognitive Function in Older Adults
I've previously discussed the synergy between magnesium and vitamin D, and the importance of vitamin D for optimal immune function and overall health — especially as it pertains to lowering your risk of COVID-19. Previous studies have also highlighted the role this duo plays in cognitive function among older adults, as well as overall mortality.
Vitamin D and Magnesium Protect Cognitive Health
One such study,1 "Association of Vitamin D and Magnesium Status with Cognitive Function in Older Adults: Results from the National Health and Nutrition Examination Survey (NHANES) 2011 to 2014," points out that vitamin D not only protects neuronal structures and plays a role in neuronal calcium regulation, but also appears to impact your risk for neurodegeneration as you grow older.
Magnesium, meanwhile, aside from being required for converting vitamin D to its active form,2,3,4 also plays a role in cognitive health, and magnesium deficiency has been implicated in several neurological disorders.
Using NHANES data from 2,984 participants over the age of 60, the researchers compared serum vitamin D status and dietary magnesium intake against cognitive function scores.
After adjusting for confounding factors, including total calorie consumption and magnesium intake, higher blood levels of vitamin D positively correlated with decreased odds of having a low cognitive function score on the Digit Symbol Substitution Test.
The same trend was found when they looked at vitamin D intake, rather than blood level. The correlation of higher vitamin D levels and better cognitive function was particularly strong among those whose magnesium intake was equal to or greater than 375 mg per day. According to the authors:5
"We found that higher serum 25(OH)D levels were associated with reduced risk of low cognitive function in older adults, and this association appeared to be modified by the intake level of magnesium."
Magnesium Improves Brain Plasticity
While magnesium intake by itself did not appear to have an impact on cognitive function in the study above, other research has highlighted its role in healthy cognition.
Memory impairment occurs when the connections (synapses) between brain cells diminish. While many factors can come into play, magnesium is an important one. As noted by Dr. David Perlmutter, a neurologist and fellow of the American College of Nutrition:6
"It has now been discovered that magnesium is a critical player in the activation of nerve channels that are involved in synaptic plasticity. That means that magnesium is critical for the physiological events that are fundamental to the processes of learning and memory."
A specific form of magnesium called magnesium threonate was in 2010 found to enhance "learning abilities, working memory, and short- and long-term memory in rats."7 According to the authors, "Our findings suggest that an increase in brain magnesium enhances both short-term synaptic facilitation and long-term potentiation and improves learning and memory functions."
COVID-19 Can Deprive Brain of Oxygen
While we're on the topic of the brain, a July 1, 2020, article8 in The Washington Post reviewed findings from autopsies of COVID-19 patients. Surprisingly, Chinese researchers have reported9 that COVID-19 patients can exhibit a range of neurological manifestations.
A June 12, 2020, letter to the editor10 published in The New England Journal of Medicine also discusses the neuropathological features of COVID-19. As reported by The Washington Post:11
"Patients have reported a host of neurological impairments, including reduced ability to smell or taste, altered mental status, stroke, seizures — even delirium … In June, researchers in France reported that 84% of patients in intensive care had neurological problems, and a third were confused or disoriented at discharge.
… Also this month, those in the United Kingdom found that 57 of 125 coronavirus patients with a new neurological or psychiatric diagnosis had experienced a stroke due to a blood clot in the brain, and 39 had an altered mental state.
Based on such data and anecdotal reports, Isaac Solomon, a neuropathologist at Brigham and Women's Hospital in Boston, set out to systematically investigate where the virus might be embedding itself in the brain.
He conducted autopsies of 18 consecutive deaths, taking slices of key areas: the cerebral cortex (the gray matter responsible for information processing), thalamus (modulates sensory inputs), basal ganglia (responsible for motor control) and others …"
Interestingly, while doctors and researchers initially suspected that brain inflammation was causing the neurological problems seen in some patients, Solomon's autopsies found very little inflammation. Instead, these neurological manifestations appear to be the result of brain damage caused by oxygen deprivation.
Signs of oxygen deprivation were present both in patients who had spent a significant amount of time in intensive care, and those who died suddenly after a short but severe bout of illness. I believe this is likely due to increases in clotting in the brain microvasculature.
Solomon told The Washington Post he was "very surprised," by the finding. It makes sense, though, considering COVID-19 patients have been found to be starved for oxygen. As reported by The Washington Post:12
"When the brain does not get enough oxygen, individual neurons die … To a certain extent, people's brains can compensate, but at some point, the damage is so extensive that different functions start to degrade … The findings underscore the importance of getting people on supplementary oxygen quickly to prevent irreversible damage."
Magnesium and Vitamin D Impact Mortality
Getting back to magnesium and vitamin D, previous research13 using NHANES data from 2001 through 2006 found the duo has a positive impact on overall mortality rates. This study also pointed out that magnesium "substantially reversed the resistance to vitamin D treatment in patients with magnesium-dependent vitamin-D-resistant rickets."
The researchers hypothesized that magnesium supplementation increases your vitamin D level by activating more of it, and that your mortality risk might therefore be lowered by increasing magnesium intake. That is indeed what they found. According to the authors:
"High intake of total, dietary or supplemental magnesium was independently associated with significantly reduced risks of vitamin D deficiency and insufficiency respectively. Intake of magnesium significantly interacted with intake of vitamin D in relation to risk of both vitamin D deficiency and insufficiency.
Additionally, the inverse association between total magnesium intake and vitamin D insufficiency primarily appeared among populations at high risk of vitamin insufficiency.
Furthermore, the associations of serum 25(OH)D with mortality, particularly due to cardiovascular disease (CVD) and colorectal cancer, were modified by magnesium intake, and the inverse associations were primarily present among those with magnesium intake above the median.
Our preliminary findings indicate it is possible that magnesium intake alone or its interaction with vitamin D intake may contribute to vitamin D status. The associations between serum 25(OH)D and risk of mortality may be modified by the intake level of magnesium."
Magnesium Lowers Vitamin D Requirement by 146%
According to a scientific review14,15 published in 2018, as many as 50% of Americans taking vitamin D supplements may not get significant benefit as the vitamin D simply gets stored in its inactive form, and the reason for this is because they have insufficient magnesium levels.
Research published in 2013 also highlighted this issue, concluding that higher magnesium intake helps reduce your risk of vitamin D deficiency by activating more of it. As noted by the authors:16
"High intake of total, dietary or supplemental magnesium was independently associated with significantly reduced risks of vitamin D deficiency and insufficiency respectively.
Intake of magnesium significantly interacted with intake of vitamin D in relation to risk of both vitamin D deficiency and insufficiency … Our preliminary findings indicate it is possible that magnesium intake alone or its interaction with vitamin D intake may contribute to vitamin D status."
More recently, GrassrootsHealth concluded17 you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
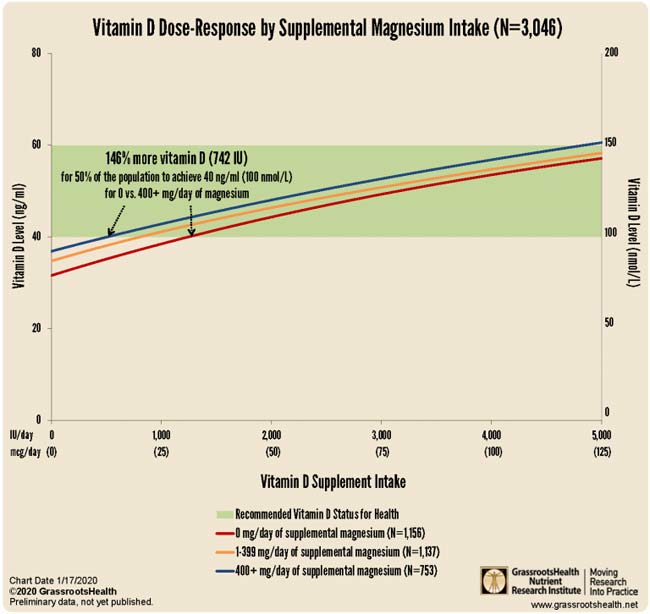
The interplay between magnesium and vitamin D isn't a one-way street, though. It goes both ways. Interestingly, while vitamin D improves magnesium absorption,18 taking large doses of vitamin D can also deplete magnesium.19 Again, the reason for that is because magnesium is required in the conversion of vitamin D into its active form.
Magnesium + Vitamin K Lowers Vitamin D Requirement Even More
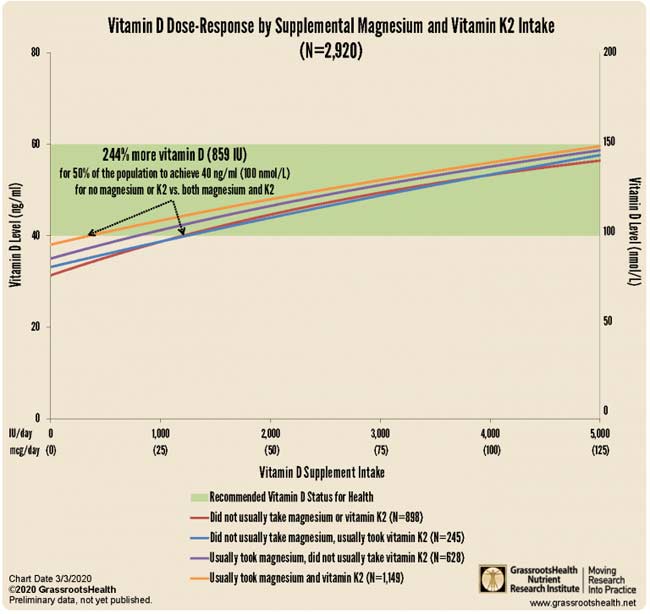
Magnesium isn't the only nutrient that can have a significant impact on your vitamin D status. GrassrootsHealth data further reveal you can lower your oral vitamin D requirement by a whopping 244% simply by adding magnesium and vitamin K2. As reported by GrassrootsHealth:20
"… 244% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental magnesium or vitamin K2 compared to those who usually took both supplemental magnesium and vitamin K2."
How to Boost Your Magnesium Level
The recommended daily allowance for magnesium is around 310 mg to 420 mg per day depending on your age and sex,21 but many experts believe you may need anywhere from 600 mg to 900 mg per day.22
Personally, I believe many may benefit from amounts as high as 1 to 2 grams (1,000 to 2,000 mg) of elemental magnesium per day, as most of us have EMF exposures that simply cannot be mitigated, and the extra magnesium may help lower the damage from that exposure.
My personal recommendation is that unless you have kidney disease and are on dialysis, continually increase your magnesium dose until you have loose stools and then cut it back. You want the highest dose you can tolerate and still have normal bowel movements.
When it comes to oral supplementation, my personal preference is magnesium threonate, as it appears to be the most efficient at penetrating cell membranes, including your mitochondria and blood-brain barrier. But I am also fond of magnesium malate, magnesium citrate, and ionic magnesium from molecular hydrogen as each tablet has 80 mg of elemental magnesium.
Eat More Magnesium-Rich Foods
Last but not least, while you may still need magnesium supplementation (due to denatured soils), it would certainly be wise to try to get as much magnesium from your diet as possible. Dark-green leafy vegetables lead the pack when it comes to magnesium content, and juicing your greens is an excellent way to boost your intake. Foods with high magnesium levels include:23
|
Avocados |
Swiss chard |
|
Turnip greens |
Beet greens |
|
Herbs and spices such as coriander, chives, cumin seed, parsley, mustard seeds, fennel, basil and cloves |
|
|
Brussel sprouts |
Organic, raw grass fed yogurt and natto |
|
Romaine lettuce |
from Articles https://ift.tt/3j7gu77
via IFTTT