Masks Delay Inevitable Acceptance of COVID-19 Reality
Nine months into the COVID-19 pandemic, the bitter conflict about mask wearing continues. In my view, the reason for this is because the science behind the mask mandates is never addressed by the politicians and public health professionals making the recommendations, and the media have completely given up on their journalistic duty.
What you end up with is Dr. Anthony Fauci saying things like "the data on mask wearing speaks for itself,"1 without telling you that virtually all studies published to date show that universal mask wearing does not prevent the spread of viral illness. The remedy would be journalistic investigation, but the mainstream media clearly doesn't fulfill that role anymore.
It's one thing to rely on opinion and unsubstantiated belief when making decisions for your own self. It's another when opinion is used to justify public health mandates. When we're talking about the health of billions of people, science really should guide the decisions made, and that means actually taking a cold hard look at the scientific literature.
A Journalist Investigates
In the featured video, Robert F. Kennedy Jr., founder of Children's Health Defense, interviews investigative journalist Jeremy Hammond, who has written extensively about foreign policy, finance, vaccines and, more recently, pandemic response measures.
In the interview, they review a range of questions, including: Where did SARS-CoV-2 come from? Is it possible that it was the result of gain-of-function research? What is the end goal of global measures such as lockdowns and universal mask wearing? Is it really all about protecting public health, or is there some other agenda at play?
With regard to mask wearing, what does the science say about their effectiveness against viral illnesses? Are there any drawbacks, such as ill health effects? Should children wear masks even though their risk of severe COVID-19 illness and death is virtually nonexistent and they're not a significant vector for spread?
What are the larger societal consequences of mask wearing? What impact do the media have on how the public perceives mask orders, and just how do the media manufacture consent for these draconian freedom-robbing measures?
As noted by Kennedy, one commonly used tactic is to claim scientific consensus; that somehow, the science is unequivocal and cannot be disputed. It's important to understand that this is nonsense. Science is never "settled," and it's exceptionally rare to end up with a scientific consensus on anything, because there are almost always two or more sides to any given inquiry.
Arguing for scientific consensus is particularly egregious and ludicrous when the bulk of the evidence actually demonstrates the complete opposite of what they say it does!
It's really nothing short of "gaslighting"2 — a term used to describe a particularly insidious form of psychological manipulation in which victims are systematically fed false information that makes them question what they know to be true. Over time, the victim becomes increasingly unable to discern truth from falsehood as they start doubting their own perceptions.
What Does the Science Say?
With regard to universal mask wearing, the bottom line, Hammond says, is that the science does not support these recommendations. Under certain conditions, in certain settings, they can be modestly helpful, but by and large, there's no support for the idea that people wearing masks everywhere they go will reduce infection rates and save lives.
Hammond points out that even the World Health Organization, in its June 5, 2020, guidance3 on face mask use, noted that there's no direct evidence that universal masking of healthy people is an effective intervention against respiratory illnesses. According to the WHO:4
"Meta-analyses in systematic literature reviews have reported that the use of N95 respirators compared with the use of medical masks is not associated with any statistically significant lower risk of the clinical respiratory illness outcomes or laboratory-confirmed influenza or viral infections …
At present, there is no direct evidence (from studies on COVID- 19 and in healthy people in the community) on the effectiveness of universal masking of healthy people in the community to prevent infection with respiratory viruses, including COVID-19."
At the time, WHO recommended that cloth masks "should only be … used by infected persons … in community settings and not for prevention."5 However, like Fauci, the WHO has vacillated on a number of measures, and in its October 20, 2020, update,6 the WHO is now back to urging people to use masks "as part of a comprehensive strategy of measures to suppress transmission and save lives."
And, despite the fact that there are no quality standards for cloth masks at all, they recommend wearing a fabric mask unless you're in a higher risk group. Medical grade masks are only recommended for those over 60, people with underlying health conditions, those who feel ill and/or those caring for an ill family member.
Policy Review Found No Support for Universal Masking
A policy review paper7 published in Emerging Infectious Diseases in May 2020 — the Center for Disease Control and Prevention's journal — also found no evidence to support universal mask wearing as a protective measure in non-health care settings. According to the authors:
"Although mechanistic studies support the potential effect of hand hygiene or face masks, evidence from 14 randomized controlled trials of these measures did not support a substantial effect on transmission of laboratory-confirmed influenza …
Disposable medical masks (also known as surgical masks) are loose-fitting devices that were designed to be worn by medical personnel to protect accidental contamination of patient wounds, and to protect the wearer against splashes or sprays of bodily fluids …
There is limited evidence for their effectiveness in preventing influenza virus transmission either when worn by the infected person for source control or when worn by uninfected persons to reduce exposure.
Our systematic review found no significant effect of face masks on transmission of laboratory-confirmed influenza … In this review, we did not find evidence to support a protective effect of personal protective measures or environmental measures in reducing influenza transmission."
Another meta-analysis and scientific review8 — which focused on randomized controlled studies rather than observational ones and was led by respected researcher Thomas Jefferson, cofounder of the Cochrane Collaboration — posted on the prepublication server medRxiv in April 2020, found that, compared to no mask, mask wearing in the general population or among health care workers did not reduce influenza-like illness (ILI) cases or influenza.
In one study, which looked at quarantined workers, it actually increased the risk of contracting influenza, but lowered the risk of ILI. They also found there was no difference between surgical masks and N95 respirators.
Jefferson also wrote an interesting article9 for the Centre for Evidence-Based Medicine (CEBM), posted July 23, 2020, in which he provides a brief review of these studies. In it, he also bemoans the fact that lack of scientific evidence is being hidden by politics.
Policy Makers Lean on Low Quality Evidence
In an October 28, 2020, Wall Street Journal opinion piece,10 Joseph Ladapo, an associate professor at UCLA's David Geffen School of Medicine, points out that "A hallmark of COVID-19 pandemic policy has been the failure of political leaders and health officials to anticipate the unintended consequences of their actions," and that includes mask mandates.
"First, consider how the debate has evolved and the underlying scientific evidence. Several randomized trials of community or household masking have been completed," Ladapo writes.
"Most have shown that wearing a mask has little or no effect on respiratory virus transmission11 … In March, when Anthony Fauci said, 'wearing a mask might make people feel a little bit better' but 'it's not providing the perfect protection that people think it is,' his statement reflected scientific consensus, and was consistent with the World Health Organization's guidance.
Almost overnight, the recommendations flipped. The reason? The risk of asymptomatic transmission. Health officials said mask mandates were now not only reasonable but critical. This is a weak rationale, given that presymptomatic spread of respiratory viruses isn't a novel phenomenon in public health …
The public assumes that research performed since the beginning of the pandemic supports mask mandates. Policy makers and the media point to low-quality evidence, such as a study of COVID-19 positive hairstylists in Missouri or a Georgia summer camp with an outbreak.
These anecdotes, while valuable, tell us nothing about the experience of other hairdressers or other summer camps that adopted similar or different masking practices. Also low-quality evidence: Videos of droplets spreading through air as people talk, a well-intended line of research that has stoked fears about regular human interactions."
Speaking of videos showing how speaking disperses potentially contaminated droplets, for each such video, there's another showing the other side of the argument. For example, the video below shows how the vapors from an e-cigarette flows right through the surgical mask. If vapor can flow through, airborne viruses do too.
Do Masks Reduce Infection Rates?
Ladapo does highlight one study published in Health Affairs in June 2020, which found that U.S. states with universal mask mandates saw a 2% reduction in growth rates of positive COVID-19 tests compared to states that did not mandate masks. Over time, even "modest reductions can translate into large differences," he notes. Maybe, maybe not. Consider what Jefferson notes in his CEBM article:12
"Norway's Institute for Public Health reported that if masks did work then any difference in infection rates would be small when infection rates are low: assuming 20% asymptomatics and a risk reduction of 40% for wearing masks, 200,000 people would need to wear one to prevent one new infection per week."
Either way, even if masks do reduce infection rates somewhat, that's still different from suggesting that universal mask wearing will bring the pandemic to an end.
"The most reasonable conclusion from the available scientific evidence is that community mask mandates have — at most — a small effect on the course of the pandemic. But you wouldn't know that from watching cable news," Ladapo writes.
"Claims that low mask compliance is responsible for rising case counts are also not supported by Gallup data,13 which show that the percentage of Americans reporting wearing masks has been high and relatively stable since June. Health officials and political leaders have assigned mask mandates a gravity unsupported by empirical research."
Now, while it may be tempting to hitch the entire pro-mask argument on that Health Affairs study, remember that good science must be reproducible, and in this case, other investigations have found states' mask rules appear to have had nothing to do with infection rates after all.
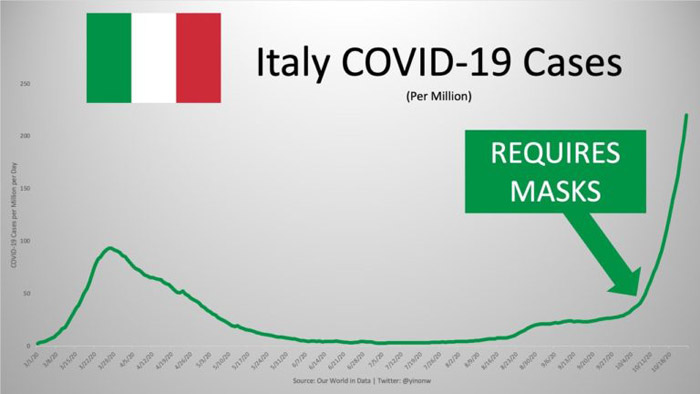
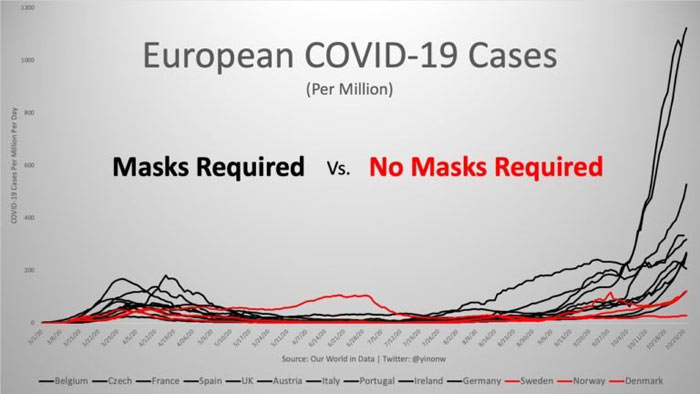
In his article14 "These 12 Graphs Show Mask Mandates Do Nothing to Stop COVID," Yinon Weiss points out that "No matter how strictly mask laws are enforced nor the level of mask compliance the population follows, cases all fall and rise around the same time." To see all of the graphs, check out Weiss' article15 or Twitter thread.16 Here are just a select few to bring home the point:



Masks Cannot Shield Us From Harsh Realities
Perhaps the least scientific recommendation of all is the rule to wear masks outdoors. A contact-tracing study17 that looked at 318 COVID-19 outbreaks involving at least three people found that just one single incident could be traced back to outdoor transmission.
"By paying outsize and scientifically unjustified attention to masking, mask mandates have the unintended consequence of delaying public acceptance of the unavoidable truth," Ladapo writes in his WSJ opinion article.18
"In countries with active community transmission and no herd immunity, nothing short of inhumane lockdowns can stop the spread of COVID-19, so the most sensible and sustainable path forward is to learn to live with the virus.
Shifting focus away from mask mandates and toward the reality of respiratory viral spread will free up time and resources to protect the most vulnerable Americans ...
Until the reality of viral spread in the U.S. … is accepted, political leaders will continue to feel justified in keeping schools and businesses closed, robbing young people of the opportunity to invest in their futures, and restricting activities that make life worthwhile."
Journals Refuse to Publish Negative Mask Study
The most recent evidence of all, which would bring us quite a bit closer to settling the argument about masks is a Danish randomized controlled trial of 6,000 people that sought to prove the usefulness of face masks against COVID-19 infection. The problem appears to be that it didn't, because the researchers can't get it published.
According to the researchers, the study will be published as soon as "someone dares to do so." Considering the argument against mask wearing has been the lack of evidence, if this COVID-19 specific trial actually shows that it works, why would journals refuse to publish it?
The controversy has been covered in a Twitter thread19 by Alex Berenson, a former New York Times reporter. A cursory translation of the study,20 which is currently only available in German, reveals that it found mask wearing resulted in tens of millions of contaminations that can occur each day as people use the masks inappropriately, touch their faces and neglect to wash their hands.
For this reason, universal mask wearing may actually do more harm than good. This is clearly important information that should be disseminated to the general public, yet medical journals are preventing that from happening. As reported by the CEBM,21 several trials are currently registered in which they are looking to assess the effectiveness of various masks against COVID-19. Time will tell what the findings will be, and if we'll ever find out about them.
Undisclosed Mask Dangers
Kennedy and Hammond also discuss evidence suggesting chronic mask wearing has its risks and may lead to other unintended health effects, such as:
• Lung damage and pathological consequences from inhaled mask fibers — One paper22,23 that has yet to undergo peer-review suggests mask fibers can pose a health risk when inhaled. According to the authors:
"If even a small portion of mask fibers is detachable by inspiratory airflow, or if there is debris in mask manufacture or packaging or handling, then there is the possibility of not only entry of foreign material to the airways, but also entry to deep lung tissue, and potential pathological consequences of foreign bodies in the lungs …
If widespread masking continues, then the potential for inhaling mask fibers and environmental and biological debris continues on a daily basis for hundreds of millions of people. This should be alarming for physicians and epidemiologists knowledgeable in occupational hazards."
• Aggravation of asthma — Another potential concern is related to the plastics used. For example, surgical masks are made of polypropylene,24 a known asthma trigger.25 If you have asthma, wearing a surgical mask could potentially worsen your condition.
• "Mask mouth" (tooth decay, gum line recession and potent bad breath) is an effect dentists around the world have raised alarm about. Dr. Rob Ramondi, a dentist and cofounder of One Manhattan Dental told the New York Post:26
"We're seeing inflammation in people's gums that have been healthy forever, and cavities in people who have never had them before. About 50% of our patients are being impacted by this."
• Hypoxia-related complaints such as fatigue, headaches, shortness of breath and anxiety.27,28
• Increased infection risk — According to Dr. Russel Blaylock, face masks "pose serious risks to the healthy," as the mask can lead to a concentration of viruses in the nasal passages where they can "enter the olfactory nerves and travel into the brain." Frequent touching of your face and mask can also increase the infection risk.
Majority of People Testing Positive Are Faithful Mask Wearers
In closing, a recent CDC analysis reveals 85% of patients testing positive for COVID-19 wore face masks "often" or "always" in the two weeks preceding their positive test. It's not a randomized controlled trial, which is the gold standard, but it does tell us that, by and large, face masks do not appear to offer very good protection. If they did, infection would favor the non-wearers.
Meanwhile, mask mandates strip us of our individual sovereignty and humanity. As noted by Hammond, mask mandates really appear to be more about teaching us to obey orders, no matter whether they make sense to anyone or not. It's about teaching compliance and, unfortunately, many who have never looked at the science aid and abet the technocratic overlords' cause by shaming those who don't comply.
I predict it is likely that, at some point in the future, a tradeoff will be offered: Mask mandates will be dropped provided everyone gets vaccinated. By then, many may be willing to take just about anything as long as they don't have to wear a mask anymore.
I would encourage you to read up on the many open questions relating to fast-tracked COVID-19 vaccines before making your decision. Overall, it seems the best way to avoid having to make such a devious trade is to engage in civil disobedience now, and go unmasked.
from Articles https://ift.tt/32Lpw3n
via IFTTT