Health, Fitness,Dite plan, health tips,athletic club,crunch fitness,fitness studio,lose weight,fitness world,mens health,aerobic,personal trainer,lifetime fitness,nutrition,workout,fitness first,weight loss,how to lose weight,exercise,24 hour fitness,
Labels
Technology
New Post
World's first agreed guidance for people with diabetes to exercise safely
from Top Health News -- ScienceDaily https://ift.tt/2HNt25o
Priming the immune system to attack cancer
from Top Health News -- ScienceDaily https://ift.tt/3jH2YWQ
Muscle pain and energy-rich blood: Cholesterol medicine affects the organs differently
from Top Health News -- ScienceDaily https://ift.tt/3muRVSs
Genomic study reveals role for hypothalamus in inflammatory bowel disease
from Top Health News -- ScienceDaily https://ift.tt/2JkWRLB
Cancer-fighting gene restrains 'jumping genes'
from Top Health News -- ScienceDaily https://ift.tt/3oDYLHb
Dumbbell Squat to Overhead Press

This is the dumbbell squat to overhead press.
The post Dumbbell Squat to Overhead Press appeared first on Under Armour.
from Under Armour https://ift.tt/2GaCEHd
High Knee Drop Lunge

This is the high knee drop lunge.
The post High Knee Drop Lunge appeared first on Under Armour.
from Under Armour https://ift.tt/3ovU16J
Picking a Cooking Oil

What is the healthiest oil to cook with?
The post Picking a Cooking Oil appeared first on Under Armour.
from Under Armour https://ift.tt/34uSWnB
What It Took for This Obese Doctor to Take His Own Health Advice

Kevin turned to food for comfort as he dealt with the death of his father. He chose a healthier path when his sister was diagnosed with cancer.
The post What It Took for This Obese Doctor to Take His Own Health Advice appeared first on Under Armour.
from Under Armour https://ift.tt/32QBnM1
Clamshell

This is the clamshell.
The post Clamshell appeared first on Under Armour.
from Under Armour https://ift.tt/31vURGD
Cut chores and kill chill time: New advice to boost children's academic achievement
from Top Health News -- ScienceDaily https://ift.tt/3jDGRAL
High-sugar diet can damage the gut, intensifying risk for colitis
from Diet and Weight Loss News -- ScienceDaily https://ift.tt/3jDlijW
High-sugar diet can damage the gut, intensifying risk for colitis
from Top Health News -- ScienceDaily https://ift.tt/3jDlijW
Denisovan DNA in the genome of early East Asians
from Top Health News -- ScienceDaily https://ift.tt/3oCXhx1
Positive outlook predicts less memory decline
from Top Health News -- ScienceDaily https://ift.tt/3mAdpgQ
Social isolation puts women at higher risk of hypertension
from Diet and Weight Loss News -- ScienceDaily https://ift.tt/3kEkNYc
Learning the language of sugars
from Top Health News -- ScienceDaily https://ift.tt/3oBnIDf
Social isolation puts women at higher risk of hypertension
from Top Health News -- ScienceDaily https://ift.tt/3kEkNYc
Younger knee replacement patients more likely to require reoperation
from Top Health News -- ScienceDaily https://ift.tt/34CgdUI
Mechanics of mucus in cystic fibrosis patients
from Top Health News -- ScienceDaily https://ift.tt/2TxpiYF
Performance test for neural interfaces
from Top Health News -- ScienceDaily https://ift.tt/31PuTOv
How the immune system deals with the gut's plethora of microbes
from Top Health News -- ScienceDaily https://ift.tt/3oFj3QE
Nudges fail more often than is reported
from Top Health News -- ScienceDaily https://ift.tt/3oLzXNR
Small brain device proves big game changer for severely paralysed patients
from Top Health News -- ScienceDaily https://ift.tt/3ox8iQm
Talking to your doctor about an abusive relationship
When Jayden called our clinic to talk about worsening migraines, a medication change was one potential outcome. But moments into our telehealth visit, it was clear that a cure for her problems couldn’t be found in a pill. “He’s out of control again,” she whispered, lips pressed to the phone speaker, “What can I do?”
Unfortunately, abusive relationships like Jayden’s are incredibly common. Intimate partner violence (IPV) harms one in four women and one in 10 men in the United States. People sometimes think that abusive relationships only happen between men and women. But this type of violence can occur between people of any gender and sexual orientation.
Experiencing abuse can be extremely isolating, and can make you feel hopeless. But it is possible to live a life free from violence. Support and resources are available to guide you toward safety — and your doctor or health professional may be able to help in ways described below.
What is intimate partner violence?
Intimate partner violence (IPV) isn’t just physical abuse like kicking or choking, though it can include physical harm. IPV is any emotional, psychological, sexual, or physical way your partner may hurt and/or control you. This can include sexual harassment, threats to harm you, stalking, or controlling behaviors such as restricting access to bank accounts, children, friends, or family.
If this sounds like your relationship, consider talking to your doctor or health care professional, or contact the National Domestic Violence Hotline at 800-799-SAFE.
What does a healthy relationship look like?
Media images show us uniformly blissful relationships, but perfect relationships are a myth. This culture can make it difficult for us to recognize unhealthy characteristics in our own relationships. Respect, trust, open communication, and shared decisions are part of a healthy relationship. You should be able to freely participate in leisure activities or see friends without fear of your partner’s reaction. You should be able to share your opinions or make decisions without fear of retaliation or abuse. Sexual and physical intimacy should include consent — meaning that no one uses force or guilt to compel you to do things that hurt you or make you feel uncomfortable.
How can a health professional help me?
Health professionals like doctors or nurses can take a history and assess how the abuse may be affecting your health, well-being, and safety. Trauma from IPV can cause visible symptoms, like bruises or scars, as well as more subtle symptoms, like abdominal pain, headaches, trouble sleeping, or symptoms of traumatic brain injury. Health professionals can also provide referrals to see specialists, if needed.
With your consent, health professionals can take a detailed history, examine you, and document the exam findings in your confidential medical record. Let them know if you are concerned that your partner will view your medical record, so measures can be taken to keep it confidential. This documentation can help to strengthen a court case if you decide to pursue legal action in the future.
Additionally, you may be at risk for pregnancy or certain sexually transmitted infections (STIs). A health professional can perform tests for STIs or pregnancy and offer birth control options. Some forms of birth control are less easily detected by your partner, like an IUD, or a contraceptive implant or injection.
Health professionals can help you develop a safety plan if you feel unsafe. They can also help connect you with social services, legal services, and specially trained advocates. If you would like, health professionals can also connect you with law enforcement to file a report.
What is a sexual assault exam?
If you have experienced sexual assault within 120 hours (five days), you may be offered a sexual assault medical examination. This exam is voluntary. It is performed by a trained health professional and may include a full body exam, including your vagina, penis, or anus. It may also include taking blood, urine, or body surface samples and/or photographs that could be used during an investigation or legal action. You may be prescribed medication that could prevent infections or a pregnancy. You can click here to learn more about the sexual assault exam.
What can I expect if I talk to a health care professional about IPV?
Health professionals should listen to you supportively and without judgement. While not all health professionals are trained in trauma-informed care, it is your right to be treated with respect and empathy to help you feel safe and empowered. You should not be pressured to do anything you don’t want to do. And this shouldn’t change the care you receive. You have the right to decline any care you are not comfortable with. You get to decide how you want to proceed after you share information with your healthcare professional, whether that means seeking out legal support, making a safety plan to leave the relationship, or choosing to stay in the relationship and be connected to ongoing support. And you can choose not to share information about abuse at all.
Will the conversation be private and confidential?
These discussions should occur with you and your health professional in a private space. If your abusive partner accompanies you to your appointment, your health professional may ask them to leave the examination room for a period of time so that you have the privacy to talk openly. You can also ask to speak with the health professional alone.
In most cases, discussing your experiences with your health professional is confidential under HIPAA. All states have laws that protect children, elders and people with disabilities from abuse of any kind. Your health professional is obligated in certain circumstances to report abuse, such as violence against a minor or vulnerable adult. However, only a few states require health professionals to report intimate partner abuse.
Where can I find more resources on IPV?
Want to learn more about IPV and how to seek help?
If you or someone you know you is at risk, call the National Domestic Violence Hotline at 800-799-SAFE (7233) or 800-787-3224. This hotline is for anyone, regardless of race, sex, ethnicity, gender identity, sexual orientation, religion, or ability.
If you are unable to speak safely, you can visit thehotline.org or text LOVEIS to 22522. They are available 24/7 by phone or with a live chat, and can work with you to find help in your area.
- RAINN (national resource for sexual assault and violence)
- Love Is Respect (national resource for dating violence)
- WomensLaw.org (legal information for women experiencing domestic violence)
- LGBT National Help Center (LGBTQ+ resources, including chat and peer counseling).
The post Talking to your doctor about an abusive relationship appeared first on Harvard Health Blog.
from Harvard Health Blog https://ift.tt/2TwTuTI
Why COVID-19 Is Not the 3rd Leading Cause of Death
According to Dr. Thomas Frieden, former director of the U.S. Centers for Disease Control and Prevention, COVID-19 is now the third leading cause of death in the U.S., killing more Americans than "accidents, injuries, lung disease, diabetes, Alzheimer's and many, many other causes."1,2
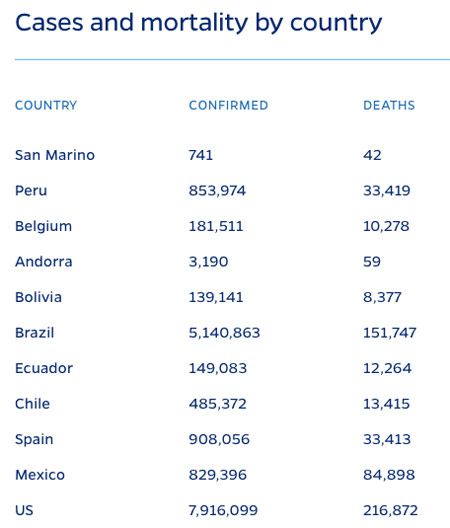
This claim is said to be based on data from Johns Hopkins University which, at the time Frieden made that statement in August 2020, reported that about 170,000 of the 5.4 million Americans who had tested positive had died.3 At the time of this writing, Johns Hopkins reports4 the U.S. has recorded 7,916,099 positive tests and 216,872 COVID-19-related deaths.
Medical Errors Dwarf COVID-19 Concerns
There are many reasons not to panic over Frieden's claim. I'll review mortality statistics in just a moment but, first, I want to highlight a leading cause of death that continues to be swept under the proverbial rug, namely medical errors, because medical errors also play a role in the death toll attributed to COVID-19.
In 2016, a Johns Hopkins study5,6 found more than 250,000 Americans die each year from preventable medical errors, effectively making modern medicine the third leading cause of death in the U.S. I reported these findings in "Medical Errors: Still the Third Leading Cause of Death."
In 2017, medical mistakes were found to affect 1 in 5 people. Common examples of medical mistakes included receiving the wrong medication, having the wrong procedure done, waking up during surgery or acquiring a hospital-related infection.
Other research7 has estimated the number of Americans dying from medical mistakes may actually be as high as 440,000. The reason for the discrepancy in the numbers is because medical errors are rarely noted on death certificates, and death certificates are what the CDC relies on to compile its death statistics.
As a result, the severity of the problem goes unnoticed. Either way, whether it's 250,000 or 440,000, medical errors still claim more lives than COVID-19 has, and it does so on an annual basis.
Medical Errors Responsible for Most COVID-19 Deaths
We also need to remember that a large portion of those who died from COVID-19 were in fact victims of medical errors. As I reported in "Nurse on the Frontlines of COVID-19 Shares Her Experience" and "Frontline Nurse Speaks Out About Lethal Protocols," Elmhurst Hospital Center in Queens, New York — which was "the epicenter of the epicenter" of the COVID-19 pandemic in the U.S. — grossly mistreated COVID-19 patients, causing their death.8
According to retired Army Sgt. Erin Olszewski, a nurse who worked at Elmhurst during the height of the pandemic, hospital administrators and doctors made a long list of errors, most egregious of which was to place all COVID-19 patients, including those merely suspected of having COVID-19, on mechanical ventilation rather than less invasive oxygen administration.
During her time there, most patients who entered the hospital wound up being treated for COVID-19, whether they tested positive or not, and only one patient survived. The hospital also failed to segregate COVID-positive and COVID-negative patients, thereby ensuring maximum spread of the disease among noninfected patients coming in with other health problems.
By ventilating COVID-19-negative patients, the hospital artificially inflated the case load and death rate. Disturbingly, financial incentives appear to have been at play. According to Olszewski, the hospital received $29,000 extra for a COVID-19 patient receiving ventilation, over and above other treatments. In August 2020, CDC director Robert Redfield admitted that hospital incentives likely elevated hospitalization rates and death toll statistics around the country.
Irresponsible State Leadership Caused Many COVID-19 Deaths
Another major error that drove up the death toll was state leadership's decision to place infected patients into nursing homes, against federal guidelines.9 According to an analysis10,11 by the Foundation for Research on Equal Opportunity, which included data reported by May 22, 2020, an average of 42% of all COVID-19 deaths in the U.S. had occurred in nursing homes, assisted living and other long-term care facilities.
This is extraordinary, considering this group accounts for just 0.62% of the population. By and large, nursing homes are ill equipped to care for COVID-19 infected patients.12 While they're set up to care for elderly patients — whether they are generally healthy or have chronic health problems — these facilities are rarely equipped to quarantine and care for people with highly infectious disease.
It's logical to assume that comingling infected patients with noninfected ones in a nursing home would result in exaggerated death rates, as the elderly are far more prone to die from any infection, including the common cold. We also learned, early on, that the elderly were disproportionately vulnerable to severe SARS-CoV-2 infection.
Yet ordering infected patients into nursing homes with the most vulnerable population of all is exactly what several Democrat governors decided to do, including New York Gov. Andrew Cuomo,13 Pennsylvania Gov. Tom Wolf, New Jersey Gov. Phil Murphy, Michigan Gov. Gretchen Whitmer and California Gov. Gavin Newsom.
ProPublica published an investigation14 June 16, 2020, comparing a New York nursing home that followed Cuomo's misguided order with one that refused, opting to follow the federal guidelines instead. The difference was stark.
By June 18, the Diamond Hill nursing home — which followed Cuomo's directive — had lost 18 residents to COVID-19, thanks to lack of isolation and inadequate infection control. Half the staff (about 50 people) and 58 patients were infected and fell ill.
In comparison, Van Rensselaer Manor, a 320-bed nursing home located in the same county as Diamond Hill, which refused to follow the state's directive and did not admit any patient suspected of having COVID-19, did not have a single COVID-19 death. A similar trend has been observed in other areas.
If it weren't for systematic medical mistreatment at certain hospitals and incomprehensible decision-making by a handful of state governors, the COVID-19 death toll may well have been negligible.
Other Considerations When Evaluating COVID-19 Death Toll
We should also remember that a) the vast majority of people died with SARS-CoV-2 infection, not from it, and b) medical treatments showing significant promise have been savagely censored and even barred from use based on falsified and seriously flawed studies.
According to groundbreaking data15 released by the CDC August 26, 2020, only 6% of the total COVID-19-related deaths in the U.S. had COVID-19 listed as the sole cause of death on the death certificate.
Six percent of 201,141 (the total death toll reported by the CDC as of October 14, 2020) is 12,068. In other words, SARS-CoV-2 infection was directly responsible for just over 12,000 deaths of otherwise healthy individuals. The remaining 94% had an average of 2.6 health conditions that contributed to their deaths.
When you add all of these factors together — the wanton mismanagement of the infection in hotspots such as New York, the decision to send infected patients into nursing homes, the fact that few healthy people died from the infection and that potential medical treatments have been and still are actively suppressed — it kind of starts to look like a manufactured crisis.
Infection Fatality on Par With the Flu
While Frieden is now stoking fears by claiming COVID-19 is the third leading cause of death, and Scientific American is calling the claim that its fatality is on par with the flu "fake news,"16 I would call your attention to research looking at the fatality ratio for the average person, excluding those residing in nursing homes and other long-term care facilities.
The September 2, 2020, article17 in Annals of Internal Medicine points out that, because many who test positive for SARS-CoV-2 remain asymptomatic it's very difficult to estimate the true infection rate, and when calculating mortality rates based on confirmed "cases" (meaning positive tests) you end up overestimating the infection fatality ratio. As explained by the authors:18
"To calculate a true infection fatality ratio, population prevalence data are needed from large geographic areas where reliable death data also exist … We combined prevalence estimates from a statewide random sample with Indiana vital statistics data of confirmed COVID-19 deaths.
In brief, our stratified random sample consisted of state residents aged 12 years and older. Known decedents and incarcerated persons were excluded. Because nursing homes were limiting residents' ability to leave and re-enter the facilities, their participation was unlikely.
Participants were tested from 25 April to 29 April 2020 for active viral infection and SARS-CoV-2 antibodies, which would indicate prior infection … We calculated the IFR by age, race, sex, and ethnicity on the basis of the cumulative number of confirmed COVID-19 deaths as of 29 April 2020, divided by the number of infections.
Although nursing home residents were not tested, they represented 54.9% of Indiana's deaths. Thus, we excluded nursing home residents from all calculations (that is, deaths and infections).
To account for all infections, we added the number of patients hospitalized with COVID-19 during the testing period and noninstitutionalized COVID-19 deaths into the denominator …
Our random-sample study estimated 187,802 cumulative infections, to which 180 hospitalizations were added. The average age among all COVID-19 decedents was 76.9 years.
The overall noninstitutionalized infection fatality ratio was 0.26% … Persons younger than 40 years had an infection fatality ratio of 0.01%; those aged 60 or older had an infection fatality ratio of 1.71%."
The estimated infection fatality rate for seasonal influenza listed in this paper is 0.8%. Other sources put it a little higher. In either case, according to this paper the only people for whom SARS-CoV-2 infection is more dangerous than influenza are those over the age of 60.
All others have a lower risk of dying from COVID-19 than they have of dying from the flu. Put another way, if you're under the age of 60, your chance of dying from the flu is greater than your chance of dying from COVID-19.
White House coronavirus task force coordinator Dr. Deborah Birx also confirmed this far lower than typically reported mortality rate when she, in mid-August 2020, stated that it "becomes more and more difficult" to get people to comply with mask rules "when people start to realize that 99% of us are going to be fine."19
In addition to COVID-19 having a lethality on par with the flu (again for the average person under the age of 60):
- Data20,21 show the overall all-cause mortality has remained steady during 2020 and doesn't veer from the norm. In other words, COVID-19 has not killed off more of the population than would have died in any given year anyway
- Several studies22,23,24,25,26,27,28,29 also suggest immunity against SARS-CoV-2 infection is far more widespread than anyone imagined
- The threshold for herd immunity appears to be far lower than previously estimated30,31,32,33,34
As reported by British Sky News,35 October 7, 2020, respected scientists are now calling for a herd immunity approach to the pandemic, meaning governments should allow people who are not at significant risk of serious COVID-19 illness to go back to normal life. As of October 18, 2020, The Great Barrington Declaration36 had been signed by 10,601 medical and public health scientists and 29,296 medical practitioners.37
Effective Treatment Protocols
At this stage in the game, there's plenty of cause for optimism. In addition to data showing COVID-19 is nowhere near as lethal as initially suspected, we now have a number of safe and effective treatments. Two that I would place toward the top of the list are:
• Nebulized hydrogen peroxide (see video above) — This is a home remedy I recommend everyone familiarize themselves with, as in many cases it can improve symptoms within mere hours. It's even been shown to be effective in the later stages of the illness.
Dr. David Brownstein, who has successfully treated over 100 COVID-19 patients with nebulized hydrogen peroxide, published a case paper38 about this treatment in the July 2020 issue of Science, Public Health Policy and The Law. He also discusses its benefits in a recent interview I did with him.
I review some of the basic science of how hydrogen peroxide works, as well as some of the studies assessing its therapeutic potential, in my April 2020 article "Could Hydrogen Peroxide Treat Coronavirus?"
• The MATH+ Protocol, developed by the Front Line COVID-19 Critical Care Working Group39 (FLCCC) — There are now MATH+ protocols40 for prophylaxis, mild symptoms that can be treated at home, and a full clinical in-hospital critical care protocol. The group has issued several updates since April 2020, so be sure to download the latest versions from the Eastern Virginia Medical School COVID Care for Clinicians site.41
Lastly, there's overwhelming evidence showing that those with adequate vitamin D levels are far less likely to test positive for SARS-CoV-2, less likely to develop symptoms if infected, and less likely to suffer complications, serious illness or death.
Overall, optimizing your vitamin D level appears to be a foundational strategy to minimize your risk. To learn more, download my vitamin D report from StopCOVIDCold.com. There, you can also find a quick COVID-19 risk quiz to help you assess your general risk.
from Articles https://ift.tt/35IV0rt
via IFTTT
Studies Prove This Root Helps You Sleep and Manage Stress
Ashwagandha (Withania somnifera) is a powerful adaptogenic herb, which means it helps your body adapt to stress1 by balancing your immune system, metabolism and hormonal systems. It is known as a multipurpose herb and was used in ancient Ayurvedic and Chinese medicine.2 The plant is native to India and a member of the Solanaceae family, along with eggplant and tomato.3
A 2020 study tested ashwagandha for its ability to promote sleep. Based on the results, the researchers believe the herb could be an alternative treatment for insomnia.4 They gathered 80 participants, 40 of whom were healthy individuals without a sleep disorder and 40 who had a known diagnosis of insomnia.
Consider Ashwagandha to Improve Your Sleep Quality
Each group was further split into two groups: one intervention and one control group. The intervention group received ashwagandha and the control group received a placebo. The participants took the supplements for eight weeks during which assessments were done to evaluate sleep parameters, sleep quality and anxiety.
The results revealed that the groups of healthy individuals and those with insomnia who were taking ashwagandha demonstrated significant improvement in the study parameters. Those who had insomnia showed the most improvement. The researchers wrote the “root extract was well-tolerated by all the participants irrespective of their health condition and age.”5
The participants took 300 milligrams (mg) twice each day of the root extract KSM-66 sold by Ixoreal Biomed.6 The same supplement was tested in another study in which the researchers found it improved quality of sleep, quality of life and mental alertness in older adults.7
The researchers in the second study suggested the root extract may be effective in the elderly population as they tolerated the supplement well and “it was reported as safe and beneficial by the study participants.”8 Kartikeya Baldwa, CEO of Ixoreal Biomed Inc., commented on the results of the newest study to a reporter from NutraIngredients:9
"Sleep is critical to be healthy, to recover from exercise and to function optimally both physically and cognitively. Ashwagandha root has been referenced for centuries for its sleep benefits. This study is the first clinical study to evaluate the effect of ashwagandha root extract on sleep quality in both healthy adults and insomnia patients and demonstrates significant positive effects on sleep quality in the participants.
The paper is published in a prestigious journal and is a valuable contribution to the scientific literature. It substantiates the use of ashwagandha root extract as an adaptogen that helps reduce anxiety and promote restful sleep."
Why Improving Your Sleep Quality Is Important
The importance of getting enough quality sleep each night cannot be overstated. You likely recognize that a good sleep schedule is a vital component of a healthy lifestyle. But, according to a survey from Mattress Firm, which revealed some disturbing facts about sleep patterns in America, getting a good night’s sleep may be challenging.10
The results showed the average adult who responded to the survey didn't get the seven to eight recommended hours of sleep each night. Of those who responded, a total of 40% said their sleep was “not very good” or “not good at all.” This may be related to the activities people reported doing in bed, which included watching TV, eating and playing video games.
But it's not only the number of hours that's important, but also the quality. Fragmented sleep can trigger chronic inflammation and contribute to mental health conditions and neurological disorders such as major depression and Alzheimer's disease.11
Fragmented sleep is also associated with atherosclerosis,12 a buildup of fatty plaque in the arteries sometimes called clogged or hardened arteries that can result in fatal heart disease.13
Experts estimate that up to 70 million people in the U.S. of all ages are plagued by sleep-related health conditions.14 They are common in both men and women and span all socioeconomic classes. The potential for being sleep deprived has risen significantly in the past 30 years, according to the American Sleep Apnea Association.
Contributing factors include digital technology and blurred lines between work and home. This may be exacerbated by the recent pandemic and an increasing number of people working remotely.
Ashwagandha Helps Lower Stress Markers
In addition to improving quality of sleep, the researchers found ashwagandha reduced the measure of anxiety in the participants.15 According to the Anxiety and Depression Association of America, there is a relationship between stress and anxiety. They define the difference as stress being a response to a threat, while anxiety is a response to the stress.16
Another study evaluated the effectiveness of a full-spectrum extract of ashwagandha root to help reduce stress and anxiety.17 Since stress can lead to poor performance and increase your risk for adverse health conditions, the researchers sought to evaluate the effectiveness of ashwagandha in adults who were known to be under stress.
They gathered 64 individuals who had a history of chronic stress. Before beginning the intervention, the participants underwent laboratory testing that included measuring serum cortisol and assessing their stress level using a standardized assessment questionnaire.
The group was randomized into a treatment group and control group. Those in the study group took 300 mg of ashwagandha root twice a day for 60 days. Analysis of the data revealed a significant reduction in stress assessment at the end of 60 days when compared to the placebo group.
People taking ashwagandha also had substantially lower serum cortisol levels. The group taking ashwagandha reported only mild adverse effects that were comparable to the placebo group. The results led the researchers to conclude that the root extract was safe and effective at improving resistance to stress and self-assessed quality of life.
A systematic literature review evaluating five human trials found similar results to the interventional study. The researchers concluded each of the five studies demonstrated ashwagandha resulted in greater improvement than a placebo when measuring anxiety or stress.18
Ashwagandha May Help Improve Nonrestorative Sleep
Nonrestorative sleep is a subjective feeling you have that your sleep had been “insufficiently refreshing.”19 This may happen despite appearing like you had slept through the night. It is one of the symptoms of insomnia that can be independent of other signs.
Difficulty with nonrestorative sleep plays an important role in medical conditions such as fibromyalgia, chronic fatigue syndrome, heart disease and obesity.20 Scientists have found it is associated with other sleep disorders such as restless leg syndrome, sleep apnea and periodic limb movement disorders.
Although it has been studied in people with sleep disturbances, one team of researchers published their study protocol and rationale to evaluate the role ashwagandha may have in nonrestorative sleep in the general population.21
Because nonrestorative sleep plays an important role in medical conditions that are linked to chronic inflammation and ashwagandha has demonstrated the ability to reduce stress and prepare for sleep, researchers hoped ashwagandha would help improve scores on a restorative sleep questionnaire given to participants taking the supplement for six weeks.
The results of the study were published in the journal Sleep Medicine. The scientists enrolled 144 individuals who completed the study and found there was a 72% improvement in sleep quality in those taking ashwagandha compared to 29% in the placebo group.22
The researchers monitored data that showed a significant improvement in sleep efficiency, time, latency and wakefulness after sleep. Quality of life scores were vastly improved in physical, psychological and environmental domains. Additionally, there were no adverse events reported.
More Benefits From Ashwagandha Include Cognitive Function
A traditional use for ashwagandha is memory enhancement, particularly the root of the plant. In 2017, a published study in the Journal of Dietary Supplements demonstrated the root extract helped improve memory and cognitive function in 50 people who had mild cognitive impairment.23
This is a slight decline in cognitive ability that is associated with an increased potential risk for developing other serious dementias, including Alzheimer's disease.24 The participants were split into two groups either receiving 300 mg of ashwagandha root extract twice a day or placebo over eight weeks.
The participants taking ashwagandha also demonstrated improvement in executive function, information-processing speed and sustained attention.25 In addition to improving function, the root extract may help slow deterioration of brain cells in people diagnosed with dementia. In one review of Ayurvedic medicines, the researchers wrote:26
“The beneficial effects of Ashwagandha root constituents in neurodegenerative diseases may be due to their neurite promoting, antioxidant, anti-inflammatory, antiapoptotic, and anxiolytic activities, as well as their ability to improve mitochondrial dysfunction and restore energy levels and increase levels of antioxidant defenses such as reduced glutathione.”
Another study engaged 20 healthy men who were randomized to receive 500 mg of encapsulated root and leaf extract of ashwagandha or a placebo for 14 days.27 They were put through a battery of computerized psychometric testing and researchers found those taking ashwagandha showed significant improvements in their reaction time, card sorting testing and choice discrimination.
Considerations and Side Effects
If you choose to consider an ashwagandha supplement, talk to your holistic health care practitioner since even natural remedies, like herbs, can interact with other medications or supplements you may be taking.
Women who are pregnant or breastfeeding should avoid ashwagandha since it can cause spasmolytic activity in the uterus that may result in a premature birth. In general, ashwagandha is associated with only mild side effects, if any, and appears to be safe for most people.
Typical dosages can range from 125 mg to 1,250 mg each day. Many of the current studies provided participants with 600 mg of root extract each day. In addition to being taken internally, ashwagandha can also be useful in topical form as an essential oil diluted with a carrier oil.
from Articles https://ift.tt/2HNQ2l6
via IFTTT
We found the best gym bags that convert into stylish weekenders
from Fitness | body+soul https://ift.tt/2HHpLok