Outpatient Treatments for COVID-19 Reviewed
Dr. Pierre Kory is one of the leaders in the movement to provide early treatment for COVID infection. Kory is a critical care physician (ICU specialist), triple board certified in internal medicine, critical care and pulmonary medicine, and is part of the Frontline COVID-19 Critical Care Alliance (FLCCC), which was among the first to publish COVID treatment guidance.
Kory spent most of his career at the Beth Israel Medical Center in Manhattan, New York, where he helped run the intensive care unit. He also had a busy outpatient practice. About six years ago, he was recruited to the St. Luke’s Aurora Medical Center in Milwaukee, Wisconsin, where he led the critical care service. “When COVID hit, I was in a leadership position,” he says. “I resigned, because of the way they were handling the pandemic.”
Treatment Options Have Been Vehemently Opposed
St. Luke’s, like most hospitals across the U.S., insisted on providing supportive care only, and Kory refused to remain in a leadership position under those circumstances. Patients were, for the first time in modern medical history, told to just suffer at home until they were near death, then go to the hospital where they were placed on deadly ventilator treatment.
“I knew there was a variety of treatments that we could use [yet] we were using nothing,” he says. Doctors were even told to not use anticoagulants, even though blood clotting was “through the roof” in many patients. “You could draw blood and actually see the blood clotting very quickly in the tubes,” he says.
Since those early days, the disease seems to have changed considerably. We don’t see the high rates of blood clotting anymore, for example, which is good news.
But for some reason, from the very start, “they were literally telling us that we needed randomized controlled trials to do anything,” Kory says, and to this day, health authorities are refusing to acknowledge any treatment protocol outside of the incredibly dangerous experimental drug remdesivir, and the experimental COVID jabs.
“People were dying, [yet] all of my ideas were getting shouted down. My superiors were showing up [to my clinical meetings] and getting me to stand down, because I was entertaining the idea that we should do this, that and the other thing, and they didn't want anything to be done.
And so, I said, ‘I'm done.’ I resigned mid-April 2020. I then went to New York for five weeks and ran my old ICU in New York.”
The Importance of Steroids in the Treatment of COVID-19
In May 2020, Kory testified before the U.S. Senate, stressing how critical it was to use steroids during the hospital phase of this infection. At that time, he was still employed by the University of Wisconsin. His resignation date had not yet happened, and they “were livid that I was speaking in public, giving my opinion.”
This is remarkable, because when you’re an expert in a field, “you're actually responsible to share your insight and expertise,” Kory says. “Yet they were very unhappy that I was doing that.”
Seven weeks later, Kory was vindicated when the British Recovery trial results came out, showing the benefits of corticosteroids. Since then, steroids have become part of standard of care in the hospital phase.
Steroids are an effective tool for reducing inflammation in general, but they appear particularly important for advanced COVID infection. I had a close friend who contracted a very serious case of COVID-19 and kept worsening despite taking everything I suggested.
He knew Dr. Peter McCullough, so he texted him and was told to add prednisone and aspirin to his current regimen. As soon as he took the prednisone, he started getting better.
As explained by Kory, this is a common experience. Importantly, the evidence shows that when used early, during mild infection, corticosteroids do more harm than good. But once you are entering into moderate illness, as soon as you start to see lung dysfunction or the need for oxygen, steroids are critical and are clearly lifesaving.
Steroids Must Be Used at the Correct Time
One of the reasons for this is because SARS-CoV-2 infection triggers a very complex cascade of inflammation. More specifically, Kory says, severe COVID-19 is a macrophage activation syndrome. It’s the hyperinflammatory macrophages (a subtype of macrophages) that end up causing organ damage. So, you want to use medicines that either suppress their activity or repolarize them into hypoinflammatory macrophages.
The key is to use the steroids at the correct time — not too early and not too late, the "Goldilocks" window. There are no hard and fast rules for that, as each patient is different, but as a rule of thumb, do NOT use it until or unless you are seeing a significant worsening of symptoms to where breathing is getting more difficult.
Kory’s outpatient protocol includes prednisone on Day 7, 8 or 9, if you’re still going downhill. It is important to NOT use it early in the course of the illness as it will actually worsen the infection by increasing viral replication.
The suggested dosage is 1 milligram of prednisone or methylprednisolone per kilogram of bodyweight. When using methylprednisolone (Medrol) (which Kory prefers, in part because lung tissue concentrations are higher than prednisone), he divides it into two daily doses. Kory does not recommend the use of dexamethasone, as it doesn’t work as well for lung disease. Yet, most doctors in the U.S. use dexamethasone if they’re using steroids at all.
The dose may be increased depending on the severity and trajectory of the infection. “I probably will either double or triple the [dose] until I can get them stable,” he says.
“Once they're off oxygen, then I taper off [the steroid] over about a week to 10 days, sometimes shorter. Depends how long they were on oxygen. If they were on it for a short time, I do a fast taper; if they were on oxygen for a longer time, I'll do a slower taper. But I don't start fully tapering until they're off oxygen.”
Anticoagulants — When to Use Them
As mentioned earlier, while early COVID-19 cases often involved severe blood clotting, that feature of the infection appears to have receded. Even when clotting occurs, it’s typically much milder than what we saw in the beginning. Still, anticoagulants can be an important component in these cases.
“What I do with coagulation is, I generally follow the D dimer on admission. D dimer is a marker of endothelial injury and clotting. In patients with normal D dimers, I'll just do routine prophylaxis doses. If it's moderately elevated, I do moderate [doses] and if it's severely elevated, I'll do full dose anticoagulants,” Kory explains.
He typically uses an anticoagulant called Lovenox. Patients are also given full-dose aspirin, unless there’s a contraindication. I suspect fibrolytic enzymes like lumbrokinase and nattokinase, which help degrade fibrin, may be a better alternative to aspirin. N-acetyl cysteine (NAC) is another potential candidate. Kory is not convinced, however:
“We have used NAC in different disease models over the years. It’s a standard treatment for acetaminophen overdose, but not for pulmonary fibrosis. In pulmonary medicine, of which I'm an expert, we had decades where we studied NAC for that. None of those studies panned out. In sepsis, it didn't really pan out.
And so, for severe disease, we think it's an effective drug and it's a good antioxidant. I think it does have anticoagulation [effects], but our opinion is that it’s generally weak. So, for the hospital phase, we think it's too weak.”
Vitamin C
Another important component is intravenous vitamin C. While some university hospitals may carry IV vitamin C, most don’t but might be able to get it from another local hospital. Importantly, the vitamin C needs to be administered within the first six hours of admittance to the ICU in order to work, and it may be similar for COVID.
This is especially true for the relatively low doses recommended by the Math+ protocol of 1,500 mg or 1.5 grams. Many outpatient natural medicine physicians will use 25 grams to 50 grams of IV vitamin C, but most hospitals will not allow this high a dose, even though it is likely that higher doses will work if you missed the early treatment window (the first six hours). So pragmatic logistics is why the Math+ protocol uses relatively low doses.
One suggestion would be to call the hospital you’re thinking of using if you ever had to be admitted for COVID and ask if they have it. If not, you can ask your doctor to order it for you and bring it to the hospital, if you or a family member are admitted for COVID or sepsis. The key, of course, is having a doctor who is willing to use it. Some aren’t.
“You should’ve seen the resistance I got. At one point, I was the director of the main ICU at the University of Wisconsin and the data was so overwhelming, I said, ‘Hey, guys, can't we just start a protocol where we just give everybody on admission IV vitamin C? What's the downside?’
Everyone started talking about kidney stones and all of this nonsense, and we have so much data to show that doesn't happen in acute illness, or in IV formulations ... I feel like I live in a cartoon of medicine, because every time I discuss something with someone, they just don't believe anything works. Because if it worked, they would be doing it. It's bizarre.”
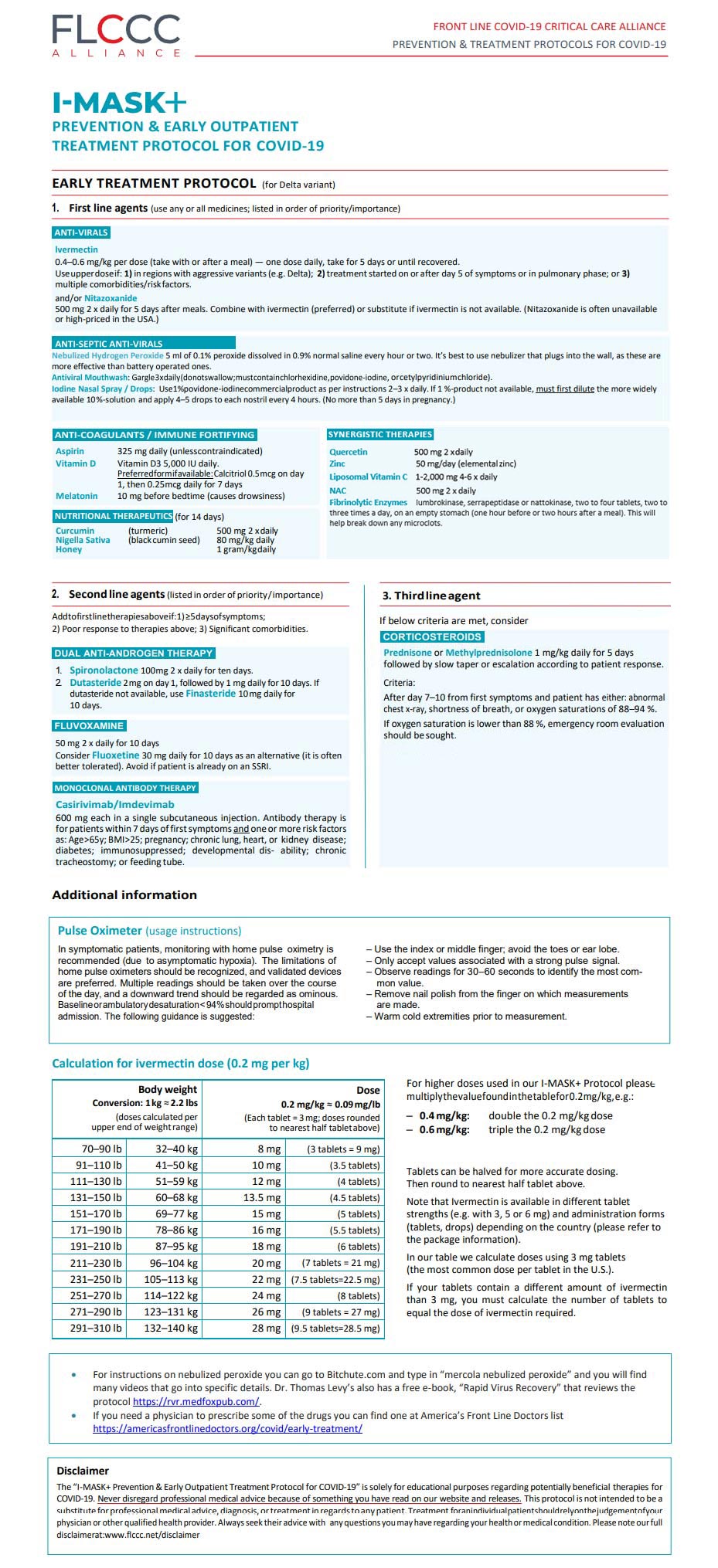
The FLCC Protocol
Sadly, the willful ignorance of many doctors is literally killing many COVID patients who could have, and should have, been saved. There’s just no doubt that protocols such as the one developed by the FLCC and the other groups listed below could have saved many, had it been widely implemented. Yet despite its success, many hospitals to this day do not use it.
“Our protocol is always evolving,” he notes. “We're not saying that this is the only way to treat it. This is how we decided to treat it. We reserve the right to deprioritize or change the dose, or substitute a new medicine.
We want to follow the data, the experience and the knowledge of this disease. That's No. 1. No. 2, all of our protocols are combination therapy protocols.
And by the way, that gives doctors fits. You know why? Because they want to know, how do you know that this is necessary? There are trials of each individual component showing that they're effective. We believe they're synergistic, but we're never going to do a trial to test every component on our protocols.
But there are a number of other protocols. The AAPS has a protocol.1 The World Council for Health,2 they have a number of options. So there are many doctors who might emphasize or de-emphasize a medicine on our protocol. And we do not pretend that ours is the only way. But we do put a lot of thought into it.
Most of our medicines are repurposed, so they're not novel. They're very well-known over decades, their safety profiles are well known, they tend to be generally low cost, and their mechanisms are well-known. A central medicine to all of our protocols — prevention, early treatment, hospital, and late phase like long-haul [syndrome] is ivermectin, for many reasons.”
Why Ivermectin?
As noted by Kory, ivermectin is a potent antiviral. “That's been demonstrated for 10 years now in the lab on a number of viruses,” he says. “They've shown that it interrupts replication of Zika, Dengue, West Nile, even HIV. And then the clinical studies are just overwhelming.” He continues:
“Can I just take one minute to say that if anyone wants to call ivermectin a controversial medicine, I just want to call out it is absolutely not controversial.
It is a medicine that is buried in corruption, and the corruption is in the suppressing of its efficacy. There are immense powers that do not want the efficacy of that drug to be known because, if it is known and becomes standard of care, it will obliterate the market for a number of novel pharmaceutical products.
When you look at the actions taken against ivermectin, it can only be understood that it's threatening something big and powerful, because boy has it been attacked [even though it’s been used in] 64 controlled trials, almost every single one of them showing benefit, many of them large benefits.
Yet they distort it to make it seem like it's controversial. It's absurd. We know it works. We know it from in vitro, in vivo animal studies, and case series.”
One of the first case series, from the Dominican Republic, was published in June 2020. They treated 3,300 consecutive emergency room COVID patients with ivermectin. Of those, only 16 went on to be hospitalized and one died. That’s pretty profound, considering these were severely ill individuals.
Importantly though, there is a dose-response relationship to the viral load. The Delta variant has been shown to produce viral loads that are 250 times higher than Alpha, and as Delta became predominant, breakthrough cases in the prevention protocol started happening.
“I'm one of them. I got COVID while I was taking it weekly,” Kory says. “Now we're doing it twice weekly. Is it the right dose? We're not sure. But we're seeing much fewer breakthroughs now on a higher dose. Could it be higher? Maybe. But, but we know it works as prevention.”
Higher doses of ivermectin are also used for treatment of Delta. In more advanced stages, the drug is useful thanks to its anti-inflammatory properties. Contrary to many other drugs, ivermectin is beneficial in all stages of the infection.
Vitamin D Optimization Is Crucial
Other components of the FLCC’s prevention and treatment protocols include products that have either antiviral or anti-inflammatory properties, or a combination thereof, such as melatonin, quercetin and zinc, and anticoagulants such as aspirin.
Ideally, everyone would optimize their vitamin D level before ever needing treatment for COVID. If you haven’t done so already, check your vitamin D blood level and if it’s below 40 ng/mL, start taking an oral supplement. Don’t wait until you’re sick. The medical literature suggests population-wide vitamin D optimization, to a level above 40 ng/mL, could have reduced COVID morbidity and mortality by about 80%.
“No question,” Kory says. “In fact ... there was a study that came out, a huge database of patients, where they looked at patients who tested their vitamin D levels before they got ill. They estimated — and they did no fancy statistical modeling logistic regression — that at 50 ng/mL, there was zero mortality.
The federal government knows that vitamin D deficiency ... is ubiquitous in nursing homes [and minorities] ... So, that we didn't have a vitamin D protocol nationally is criminal. Literally, it's criminal.”
In the hospital treatment protocol, the FLCCC recommends using calcitriol, 0.5 micrograms on Day 1 and 0.25 mcg daily thereafter for six days. Calcitriol is the active form of vitamin D typically produced in your kidneys.
This is because merely taking regular oral vitamin D fails in acute conditions as it takes weeks to be metabolized to its active form. Calcitriol is the active form, so it will start to work immediately. One can also take the vitamin D, though, as eventually adequate blood levels will be reached and the calcitriol can be discontinued.
Why Men Do Worse than Women in COVID
As mentioned earlier, the protocol also includes a number of nutraceuticals, such as quercetin and zinc. Another drug that looks promising is fluvoxamine, an antidepressant. Kory says:
“The studies continue to pan out, and even clinically, some of my colleagues who incorporated ivermectin with fluvoxamine saw much less treatment failures. I rank it as highly effective, but it doesn't cure everybody. They saw an occasional treatment fail and they said it really disappeared once they use the combo.
For someone older or with more advanced disease, more comorbidities, obese patients, diabetics, I tend to throw the kitchen sink at those folks. I try to use as many elements in the protocol as I can. So there, I’ll add fluvoxamine.
The game changer now is antiandrogens. We use spironolactone, which is a potassium-sparing diuretic, at doses above 100 mg a day. It has potent antiandrogen properties, as well as dutasteride, a 5-alpha reductase inhibitor, which also suppresses testosterone.
Androgens seem to be a huge potential driver of this illness, not only in terms of driving viral replication, but also in potentially aiding inflammation ... The trials on that are really, really potent ... so, we have an antiandrogen aspect. I've been using that on some of my older or more advanced disease patients. I'll add that on pretty quick.”
Home Treatment Recommendations for COVID
While it can be difficult to find a doctor who is willing to actually treat COVID-19 with the FLCCC protocol (or any other for that matter), many of those who are willing are making full use of telemedicine.
You can find a listing of doctors who can prescribe ivermectin and other necessary medicines on the FLCCC website. There, you can also find downloadable PDFs in several languages for prevention and early at-home treatment, the in-hospital protocol and long-term management guidance for long-haul COVID-19 syndrome. Three other protocols that have great success are:
This is a load of information to review, especially if you are fatigued and sick with COVID or have a family member struggling. So, I reviewed all the protocols and believe the FLCCC one is the easiest and most effective to follow. I’ve posted it below.
However, I’ve altered some of the dosages, and added a few more therapies that they have yet to include, such as:
|
Nebulize hydrogen peroxide 5 ml of 0.1% peroxide dissolved in 0.9% normal saline every hour or two. It’s best to use nebulizer that plugs into the wall, as these are more effective than battery operated ones. |
|
Intravenous ozone administered by a trained ozone physician. |
|
NAC 500 mg twice a day. |
|
Make sure the honey is raw honey, not normal honey from the grocery store. Raw honey can be obtained online or at a health food store. |
|
Fibrinolytic enzymes like lumbrokinase, serrapeptidase or nattokinase, two to four tablets, two to three times a day, on an empty stomach (one hour before or two hours after a meal). This will help break down any microclots. |
|
Decrease zinc dose from 100 mg to 50 mg elemental zinc, but only for three days, then decrease to 15 mg elemental zinc. |
|
Increased quercetin from 250 mg to 500 mg. |
|
Change vitamin C to liposomal C 1,000 to 2,000 mg four to six times per day. |
from Articles https://ift.tt/3s05u2q
via IFTTT
 A new study is causing fresh doubts about the safety of genetically modified crops. The research found Bt toxin, which is present in many GM crops, in human blood.
A new study is causing fresh doubts about the safety of genetically modified crops. The research found Bt toxin, which is present in many GM crops, in human blood.