Health, Fitness,Dite plan, health tips,athletic club,crunch fitness,fitness studio,lose weight,fitness world,mens health,aerobic,personal trainer,lifetime fitness,nutrition,workout,fitness first,weight loss,how to lose weight,exercise,24 hour fitness,
Labels
Technology
New Post
Scientists regenerate neurons in mice with spinal cord injury and optic nerve damage
from Top Health News -- ScienceDaily https://ift.tt/2Ss38qC
Children who have difficult relationships with their moms are clingy towards teachers
from Top Health News -- ScienceDaily https://ift.tt/2zNvNzR
Better understanding of nature's nanomachines may help in design of future drugs
from Top Health News -- ScienceDaily https://ift.tt/2y6htSI
Get your heart rate up with Kayla Itsines’ ultimate lounge-room workout
from Fitness | body+soul https://ift.tt/3f73Y5z
A vegan Snickers cheesecake that just tastes too good to be healthy
from Nutrition | body+soul https://ift.tt/2Ylfp3H
High cost of cancer drugs not always justified
from Top Health News -- ScienceDaily https://ift.tt/2xmmBS3
Mind-controlled arm prostheses that 'feel' are now a part of everyday life
from Top Health News -- ScienceDaily https://ift.tt/3f66CZx
This Visceral Tissue Affects How You Think
You may know visceral fat by another name — belly fat. In fact, it goes by several names such as "beer belly" and "middle-age spread." While many see it as an aesthetic problem, carrying extra weight in your midsection has a significant effect on your physical health, including your brain.
You have two basic types of fat. Subcutaneous fat is found just under the skin and is the type that jiggles and dimples. Visceral fat is found under the abdominal muscle, wrapped around your internal organs. This type is more dangerous as it's linked to the production inflammatory cytokines and is considered biologically active.1
Visceral fat also increases insulin resistance and your risk for metabolic syndrome. It plays a role in the development of Type 2 diabetes, heart disease, breast cancer, colorectal cancer and Alzheimer's disease.2
While many consider their body mass index (BMI) as an indication of whether they fall into a category of overweight or obesity, it is your waist measurement in combination with your waist-to-hip ratio that is a better indication of health.
This measurement of visceral fat helps predict your potential risk for chronic disease and even mortality. Where fat deposits on your body has a distinct impact on your health. Deposits in the hips and thighs result in a pear shape that has a lower potential risk for chronic disease than those with fat deposits in the abdomen, described as an apple shape.
Visceral Fat Associated With Dementia
One of the first studies3 in which researchers evaluated the association between belly fat and dementia was published in 2008. An analysis was conducted of 6,583 people in Northern California. Abdominal measurements were taken and 36 years later researchers looked for recorded diagnoses of dementia in the participants.
Of the cohort, 15.9% were diagnosed with dementia. Researchers compared those with lowest abdominal girth against the highest and found the highest had a three-fold increased risk.
In the past decade the terms "normal weight metabolic obesity," "skinny fat" and "normal weight obesity" have been used to describe those who have a normal BMI but have metabolic characteristics of being obese.4 These individuals carry excess belly fat.
One of the risks associated with a high waist-to-hip ratio, even when having a normal weight, is declining cognitive function. But not all studies yield straightforward results linking the two conditions. In a cross-sectional autopsy study,5 researchers evaluated 234 participants with abdominal visceral fat measured on autopsy.
They looked for associations between visceral fat and cognitive impairment as defined by clinical dementia. What they found were those who had higher amounts of central obesity had a lower risk of dementia later in life.
Although the authors of other studies found a relationship between obesity and cognitive impairment, the researchers expected those findings since the measurements were made at the same time and the samples were mainly of older adults. In past studies scientists have demonstrated a link between obesity and a higher risk of cognitive function decline, yet when measured later in life the results are conflicting.
The researchers reported on several studies that used a direct measurement of abdominal visceral fat and had demonstrated the same relationship found in this study. In one, a significant reduction in BMI later in life increased the risk of developing dementia in the following three years by 118%.
Study Finds a Pathway That Visceral Fat Affects Cognition
It's not enough to know a link exists. Scientists also want to know what happens at a molecular level. Researchers from Augusta University recently published a study6 that showed, for the first time, one pathway visceral fat may use as it damages your brain cells.
The effect influences the microglia, or immune cells in the brain, to change behavior and then trigger functional damage to your neurons.7 The results are important, as one of the researchers commented in a press release from the University:8
"We have moved beyond correlations saying there is a lot of visceral fat here, and there is cognitive decline here so they may be interacting with each other. We have identified a specific signal that is generated in visceral fat, released into the blood that gets through the blood brain barrier and into the brain where it activates microglia and impairs cognition."
The signal is a proinflammatory protein called interleukin-1 beta that doesn't often enter the brain. However, visceral fat "generates high, chronic levels of the signal that in turn over-activate the usually protective microglia, the resident immune cells in our brain." Research has demonstrated these reactions were problematic and this offers evidence as to how they are triggering problems.
Using an animal model, the researchers studied the effect on cognitive function and inflammation. These findings help to add pieces to the puzzle of how interleukin-1 beta may affect actions in the central nervous system.
Bigger Belly Predicts Heart Disease Better Than BMI
After a lifetime of exposure to pathogens and toxins, a weakened and overactive immune system may trigger chronic inflammation.9 When the inflammatory response triggered by visceral fat is added to this burden it may be a better predictor of heart health than your overall weight. This means those who are normal weight with visceral fat carry a greater risk than they may imagine.
Two studies that were released almost simultaneously revealed similar results — those who carry a spare tire have a greater risk of heart failure or heart disease. The first from the Norwegian University of Science and Technology was a meta-analysis of 23 studies with 650,000 participants. They looked at BMI and the risk of heart failure, finding the risk rose 41% with a rise of five BMI units and accelerated with greater weight gain.10
Those who were obese had a risk two to three times greater than their normal weight counterparts. The researchers also noted for every 10 centimeters (approximately 4 inches) of an increase in a participant's waist measurement, there was a 29% increased risk of heart failure.
The leaders of several of the studies had adjusted for factors that affect heart health, such as high blood pressure, diabetes and a poor lipid profile, but those with a higher waist circumference continued to have a greater correlation. One of the scientists from the study commented:
"Overweight individuals had a 35 per cent increased risk of heart failure as compared with normal weight individuals, and our findings indicate that overweight should be considered a clear risk factor for heart failure. Several studies have shown increased concentrations of inflammatory substances in the blood of people with abdominal obesity, and these substances are linked to increased risk of heart failure."
The second study from the Intermountain Medical Center Heart Institute and Johns Hopkins Hospital evaluated the risks of central obesity as a predictor of heart disease in those also suffering Type 1 or Type 2 diabetes without previous symptoms of heart disease.11
The team started with 200 participants who met the criteria and discovered that independent of total body weight, central obesity "was strongly associated with regional left ventricular dysfunction, which is a common cause of heart disease, including congestive heart failure."
The results were presented at the 2016 American College of Cardiology Scientific Session. The co-director of research from Intermountain Medical Center Heart Institute, Dr. Brent Muhlestein, commented on the results of the study and the implications it has on assessment and treatment.12
"Our research examined patients with diabetes, who are considered high risk for developing heart disease already, and found that the shape of your body determined if you were at a greater risk to develop left ventricular dysfunction. This study confirms that having an apple-shaped body — or a high waist circumference — can lead to heart disease, and that reducing your waist size can reduce your risks."
Stomach Fat Affects Mental Health
Visceral adipose tissue is also linked to mental health conditions such as depression and anxiety. In one study of postmenopausal women, those with abdominal obesity were more likely to struggle with depression than those without. This led the researchers to conclude that "visceral fat accumulation was an independent and positive factor significantly associated with the presence of depressive symptoms."13
Men also suffer from a higher risk of depression with abdominal obesity, as demonstrated by a study of 2,502 men and women. The researchers measured leptin levels and visceral fat and used either an assessment scale or antidepressant prescription to measure depression.14 They found higher levels of leptin increased the risk of depression in men, leading this team to conclude:
"In older men, high leptin was associated with an increased onset of depressive symptoms especially in the presence of abdominal obesity, suggesting that underlying leptin resistance may play a role in this link.
Differences in visceral fat levels and metabolic consequences may explain the absence of this association in women. These findings suggest a potential biological link between depression, obesity and their joint association with negative health outcomes."
The link between abdominal obesity and depression may be related to the inflammatory response the active fat triggers. Inflammation has a link to depression as demonstrated in several studies. In a literature review15 of 30 studies with 1,610 participants, researchers found anti-inflammatory agents reduced symptoms of depression when compared to a placebo.
These results support other evidence finding a link between inflammation and depression.16,17 Unfortunately, mental health screening may overlook this factor.
Evaluate Your Risk With Waist-to-Hip Ratio
As demonstrated in this short video, using a waist-to-hip ratio is a more reliable indication of your future risk of chronic disease, heart disease and mental health. A higher ratio is suggestive of more visceral fat accumulation around your abdominal organs, which is far more hazardous to your health than the subcutaneous fat located directly under your skin.
To determine your waist-to-hip ratio you'll want to measure both areas. Start by measuring your waist using a spring-loaded or cloth tape measure. Find your waist, which is your midpoint between your last rib and your iliac crest. These are the bones on the front of your abdomen, as shown in this video.
Measure the area in the middle without pulling the tape measure too tight. Take a couple of measurements, allowing 30 seconds between each one to allow your skin and subcutaneous tissue to return to normal. Be sure to take the measurement at the same place each time. Using just your waist circumference, your risk categories are:
| Risk Category | Female | Male |
|---|---|---|
|
Very Low |
<27.5 in (<70 cm) |
<31.5 in (<80 cm) |
|
Low |
27.5 - 35.0 in (70-89 cm) |
31.5 - 39 in (80-99 cm) |
|
High |
35.5 - 43.0 in (90-109 cm) |
29.5 - 47 in (100-120 cm) |
|
Very High |
>43.5 in (>110 cm) |
>47 in (>120 cm) |
Your hip measurement is taken at the widest part of your buttocks, again without pulling the tape too tightly and taking at least two measurements for accuracy. You get your ratio by dividing your waist measurement by your hip measurement. These are the waist-to-hip ratio norms:
| Waist-to-Hip Ratio | Men | Women |
|---|---|---|
|
Ideal |
0.8 |
0.7 |
|
Low Risk |
<0.95 |
<0.8 |
|
Moderate Risk |
0.96 - 0.99 |
0.81 - 0.84 |
|
High Risk |
>1.0 |
>0.85 |
Approaches to Addressing Belly Fat
As I've written before, doing spot reducing exercises won't burn through subcutaneous or abdominal fat. You may build strong core muscles, but they'll still be hidden under subcutaneous fat. People use the term "spot reduction" to refer to the idea you can affect layers of fat in one area of the body by exercising muscles in that area.
Visceral fat is more dangerous than subcutaneous fat but is also easier to gain and to lose. Along with practicing intermittent fasting and eating a ketogenic diet to support your mitochondrial health and weight loss efforts, these strategies may help you lose both subcutaneous and visceral fat:
• Reduce stress — Located on top of each kidney are your adrenal glands. Cortisol is a steroid produced by these glands related to your "fight or flight" response.
When you're under chronic stress cortisol increases fat distribution to your abdominal area.18 Consider some of the steps in my article, "How Stress Affects Your Body, and Simple Techniques to Reduce Stress and Develop Greater Resilience."
• Stay hydrated — Drinking water may be one of the easiest ways to reduce psychological and physical stress. Your body is made of more than 60% fluid and your kidneys require fluids to flush toxins from your body. When you're dehydrated it affects the release of cortisol and alters metabolism.19 You'll know you're well hydrated by the color of your urine, which should be light straw-colored.
• Quality sleep — Maintaining adequate amounts of quality sleep will help you control stress. Loss of sleep may alter your production of hormones, including cortisol, and leave you vulnerable to the effects of daily stress. Sleep deprivation may lead to an increase in cortisol20 leading to a compromised immune system and disruption in metabolism and cognitive impairment.
• Control insulin level — Your body produces insulin in response to eating carbohydrates, which works with cortisol to help regulate your blood sugar levels.21 By reducing your carbohydrate intake you'll reduce your insulin secretion and may help reduce the accumulation of visceral fat.
• Optimize vitamin C — Vitamin C offers resilience against stress22 and plays a role in stabilizing blood sugar, which contributes to the production and release of cortisol. When you eat multiple servings of vegetables and fruit each day, you help maintain your levels of vitamin C. Remember, fresher produce tends to have higher concentrations of vitamins.
from Articles https://ift.tt/3cYjrTN
via IFTTT
Is the Buddhist Diet the calm we all need right now?
from Nutrition | body+soul https://ift.tt/2xlgD3T
Computational techniques explore 'the dark side of amyloid aggregation in the brain'
from Top Health News -- ScienceDaily https://ift.tt/3d1BNU0
Ultra-precision nano-sensor could detect iron disorders
from Top Health News -- ScienceDaily https://ift.tt/2Wckx7v
COVID-19 crisis: Millions of US workers at risk of infections on the job
from Top Health News -- ScienceDaily https://ift.tt/2zLHO97
Brain insulin sensitivity determines body weight and fat distribution
from Diet and Weight Loss News -- ScienceDaily https://ift.tt/2Ypv7e2
Feeling burned out? The contributors could be more related to depression than you think
from Workplace Health News -- ScienceDaily https://ift.tt/2SjCVug
via IFTTT
COVID-19 crisis: Millions of US workers at risk of infections on the job
from Workplace Health News -- ScienceDaily https://ift.tt/2zLHO97
via IFTTT
F45-approved green goddess bowl is the ideal minimal-effort WFH lunch
from Nutrition | body+soul https://ift.tt/3d1dMfS
Novel imaging application illuminates processes in cancer, COVID-19
from Top Health News -- ScienceDaily https://ift.tt/2VNnrk6
Navigating the clean energy transition during the COVID-19 crisis
from Top Health News -- ScienceDaily https://ift.tt/2KILWbR
Implant-free optogenetics minimizes brain damage during neuronal stimulation
from Top Health News -- ScienceDaily https://ift.tt/3bSEbfq
Bone proteomics could reveal how long a corpse has been underwater
from Top Health News -- ScienceDaily https://ift.tt/35frl8y
Feeling burned out? The contributors could be more related to depression than you think
from Top Health News -- ScienceDaily https://ift.tt/2SjCVug
Model can predict hospital resilience for natural disasters, pandemics
from Top Health News -- ScienceDaily https://ift.tt/2xlc3mn
Molecular switch plays crucial role in learning from negative experiences
from Top Health News -- ScienceDaily https://ift.tt/3aO5G8E
How to make your at-home, pod-machine coffee taste infinitely better
from Nutrition | body+soul https://ift.tt/2KN2j7i
Mum’s genius hack to keep bread fresh for days is going viral
from Nutrition | body+soul https://ift.tt/2SkqtKS
Arteries respond in opposite ways for males and females
from Women's Health News -- ScienceDaily https://ift.tt/35jv0SJ
Arteries respond in opposite ways for males and females
from Top Health News -- ScienceDaily https://ift.tt/35jv0SJ
Schizophrenia related to abnormal fatty metabolism in the brain
from Top Health News -- ScienceDaily https://ift.tt/2Ymvjeb
Major trial shows breast cancer drug can hit prostate cancer Achilles heel
from Top Health News -- ScienceDaily https://ift.tt/2YkR1PI
ALDI launches a neck and shoulder massager soothe your WFH pains
from Fitness | body+soul https://ift.tt/2W6DyIC
Memory misfires help selfish maintain their self-image
from Top Health News -- ScienceDaily https://ift.tt/3bQpbPc
A milder hair dye based on synthetic melanin
from Top Health News -- ScienceDaily https://ift.tt/2YgGF3j
Sensitive new test detects antibodies against SARS-CoV-2 in only 10 minutes
from Top Health News -- ScienceDaily https://ift.tt/3bQF6gD
Stark disparities in COVID-19 hospitalization and death rates among New York
from Top Health News -- ScienceDaily https://ift.tt/2VOXvVo
Offspring may inherit legacy of their father's Toxoplasma infection
from Top Health News -- ScienceDaily https://ift.tt/3f2wLbE
Link identified between dietary selenium and outcome of COVID-19 disease
from Top Health News -- ScienceDaily https://ift.tt/2YhjdTF
NIH clinical trial shows remdesivir accelerates recovery from advanced COVID-19
from Top Health News -- ScienceDaily https://ift.tt/2SnaxYe
First randomized trial of remdesivir suggests antiviral drug is not associated with significant clinical benefits, more research needed
from Top Health News -- ScienceDaily https://ift.tt/2yaINPy
Researchers help give robotic arms a steady hand for surgeries
from Top Health News -- ScienceDaily https://ift.tt/3f4TbZB
To prevent antimicrobial resistance, vaccinate the world's kids
from Top Health News -- ScienceDaily https://ift.tt/3cYefPJ
Simple 'sniff test' reliably predicts recovery of severely brain injured patients
from Top Health News -- ScienceDaily https://ift.tt/3bTd9EQ
Harvard Health AdWatch: An arthritis ad in 4 parts
Perhaps you’ve grown as weary as I have of repeated arthritis ads. They appear in frequent rotation on television, online, and in magazines, promoting Enbrel, Humira, Otezla, Xeljanz, and others.
If you’ve actually read or listened to these ads, you might have felt perplexed at certain points. Here’s a quick rundown on what they’re saying — and not saying — in one of those ads.
“The clock is ticking”
Part 1: A teakettle whistles on the stove and a disembodied voice speaks as this ad for Humira opens. “This is your wakeup call. If you have moderate to severe rheumatoid arthritis, month after month the clock is ticking on irreversible joint damage. Ongoing pain and stiffness are signs of joint erosion.” Three people are shown starting their day in pain: one rubs his knee and grimaces, another has a sore shoulder, and the third, sore hands. Their suffering is clear, and you hear ticking in the background as a digital clock clicks forward one minute.
Part 2: “Humira can help stop the clock.” A garage door opens and out comes the man with the achy knee, now smiling and comfortably walking out into the sunshine as the music swells. “Prescribed for 15 years, Humira targets and blocks a source of inflammation that contributes to joint pain and irreversible damage.”
Part 3: The long list of side effects is voiced while happy scenes and beautiful music distract you: an adorable dog hikes with its once-achy-kneed owner; a young mother drops off her kids with a beaming grandma who previously was wringing her sore hands. “Humira can lower your ability to fight infection. Serious and fatal infections including tuberculosis and cancers, including lymphoma, have happened, as have blood, liver, and nervous system problems, serious allergic reactions, and new or worsening heart failure. Tell your doctor if you’ve been to areas where certain fungal infections are common, and if you’ve had tuberculosis, hepatitis B, are prone to infections, or have flulike symptoms or sores. Don’t start Humira if you have an infection.”
Part 4: The big finish is short and to the point: “Help stop the clock on irreversible joint damage. Talk to your rheumatologist.”
What did the ad get right?
Let’s start with several accurate points:
- The prolonged morning stiffness depicted at the start is a typical symptom of rheumatoid arthritis (RA). It’s so characteristic that it helps doctors make the diagnosis.
- Humira is a brand name of adalimumab, a treatment for rheumatoid arthritis and related conditions. It’s often highly effective and has a good safety profile, despite the long disclaimer about side effects.
- The drug targets inflammation. It does this by blocking tumor necrosis factor (TNF), a substance directly involved in rheumatoid arthritis inflammation. Anti-TNF drugs were first approved by the FDA for rheumatoid arthritis more than 20 years ago. They have revolutionized treatment for this disease.
- An active lifestyle is a reality for many people with rheumatoid arthritis who begin effective treatment soon after symptoms begin. The potential for improvement is often underestimated, perhaps because it wasn’t long ago that doctors had few effective options to treat rheumatoid arthritis. Fortunately, that has changed.
Now, about the rest of the ad
- Ongoing pain and stiffness are not specific signs of joint erosion. They are symptoms of joint inflammation, which may, over time, lead to erosions. However, not everyone with RA experiences joint erosions, and it generally takes many weeks or months for erosions to develop. Showing a clock with minutes ticking by implies more urgency than is accurate.
- The word “irreversible” is stated three times in this 60-second ad. While it’s true that joint damage related to RA generally does not heal, some people have minimal or no damage, especially when taking effective treatment. The implication that permanent joint damage is inevitable seems overly dramatic to me, and perhaps alarmist.
- The FDA requires that long disclaimer. While it lists the most important risks and side effects of the drug, some of its equivocal language is chosen carefully: “Serious and fatal infections… and cancers… have happened.” Were these problems caused by adalimumab? Or were they unrelated? Or do they just not know? Generally, the safety profile of anti-TNF drugs is considered good. The most recent studies suggest that there is no significant increased risk of cancer, except for skin cancers.
- I would bet that the average person seeing this ad has no idea if they’ve been in places where “certain fungal infections are common” — or what that even means! In fact, it refers to certain infections that can become silent in the body, but re-activate in people taking adalimumab. This includes histoplasmosis (Midwest of the US), Coccidioides (southwestern US), and blastomycosis (Ohio and Mississippi River Valleys and the Great Lakes).
What’s left unsaid?
The ad never mentions some important information about adalimumab:
- It’s expensive. While insurance may cover most or all of the cost, the price of adalimumab can run about $40,000/year.
- It’s given by injection under the skin (a bit like insulin injections for people with diabetes), usually every two weeks.
- Humira is only approved — and likely to work — for a few arthritic conditions, including RA. It’s not for osteoarthritis, the most common type of arthritis, an age-related, degenerative joint disease.
- Four other medications work in a similar way, with similar effectiveness and similar cost, side effects, and risks. Additionally, a host of other medications unrelated to TNF inhibition are also just as effective.
The bottom line
As drug ads go, those for arthritis in general and adalimumab in particular are not the worst I’ve seen. But they can be misleading, perplexing, and incomplete. Of course, the main purpose of these ads is to sell drugs, not to provide a complete and balanced review of treatment options for RA. You’ll need to ask your doctor for that.
Follow me on Twitter @RobShmerling
The post Harvard Health AdWatch: An arthritis ad in 4 parts appeared first on Harvard Health Blog.
from Harvard Health Blog https://ift.tt/2YsIs5J
Higher thrombus risk in men with obesity in adolescence
from Top Health News -- ScienceDaily https://ift.tt/3bOF6xt
Ultraprocessed Food Makes You Vulnerable to COVID-19
As the world deals with the scope of the COVID-19 pandemic, scientific articles have zeroed in on who is most vulnerable to the virus. It appears those who are elderly, overweight and suffer from an underlying health condition like diabetes or high blood pressure are most at risk. But the consumption of ultraprocessed food is increasingly seen as a risk factor for contracting COVID-19, too.
Ultraprocessed foods increase the risk of conditions like obesity, cancer, Type 2 diabetes, cardiovascular disease and gallstones, which make you more vulnerable to illnesses like COVID-19. In fact, eating over four servings of ultraprocessed foods daily increased the risk of premature death by 62% in a 2019 study.1
When it comes to fighting off COVID-19, ultraprocessed foods pose another health danger: They compromise the gut microbiome, which has a crucial role in your body’s immune response to infection and in maintaining overall health. Even before the virus that causes COVID-19 surfaced, ultraprocessed foods were a bad idea but during the current pandemic they are especially dangerous.
Beware of Ultraprocessed Foods
What are ultraprocessed foods, sometimes referred to as UPFs? According to the NOVA Food Classification system, designed by the Center for Epidemiological Studies in Health and Nutrition, they are:2
"[I]ndustrial formulations made entirely or mostly from substances extracted from foods (oils, fats, sugar, starch, and proteins), derived from food constituents (hydrogenated fats and modified starch), or synthesized in laboratories from food substrates or other organic sources (flavor enhancers, colors, and several food additives used to make the product hyper-palatable).
Manufacturing techniques include extrusion, moulding, and preprocessing by means of frying. Beverages may be ultra-processed."
Ultraprocessed foods, aggressively marketed by giant food producers for their profitable potential, constitute around 25% to 60% of daily energy intake in many countries, according to Science Daily. They include:3
"… packaged baked goods and snacks, fizzy drinks, sugary cereals, ready meals containing food additives, dehydrated vegetable soups, and reconstituted meat and fish products — often containing high levels of added sugar, fat, and/or salt, but lacking in vitamins and fiber."
While it is tempting to dismiss the dangers of UPFs by saying that all foods, to some extent, are "processed," food writer Bee Wilson says that is not the case:4
"UPFs are different. They are processed in ways that go far beyond cooking or fermentation, and they may also come plastered with health claims. Bettina Elias Siegel the author of Kid Food: The Challenge of Feeding Children in a Highly Processed World … 'there’s a huge difference between a cooked carrot and a bag of industrially produced, carrot-flavoured veggie puffs' …"
Moreover, cautions Wilson, food giants deliberately mislead consumers. When fat was misleadingly considered the cause of obesity, she says, the food industry rolled out low-fat products. When sugar became the culprit, food giants manipulatively marketed artificially sweetened drinks.5
UPF manufacturers have also launched successful campaigns to convince the public that obesity is not caused by their products, but by lack of exercise. Coca-Cola is among them, and, toward that end, has provided funding to universities and a wide spectrum of medical groups including the American Heart Association, the American Lung Association, the American College of Cardiology and the American Academy of Pediatrics.6
You can't help but wonder if that is why Harvard Medical School/Partners in Health, a recipient of Coca-Cola funding, writes this about obesity:7
"Obesity results from energy imbalance: too many calories in, too few calories burned. A number of factors influence how many calories (or how much ‘energy’) people burn each day, among them, age, body size, and genes. But the most variable factor — and the most easily modified — is the amount of activity people get each day."
Obesity is increasingly linked to serious cases of COVID-19 that require hospitalization, even among young people, according to The New York Times.8 The reasons are not entirely clear, but abdominal obesity can cause compression of the lungs and diaphragm, which impairs breathing ability.
Other factors that could explain the link between obesity and serious cases of COVID-19 could include pre-existing respiratory conditions, a greater amount of circulating, pro-inflammatory cytokines and low-grade inflammation, which are all correlated with obesity. Almost 80 million Americans — 42 percent of the population — are obese.9
A report released by the Intensive Care National Audit and Research Centre on 196 patients critically ill with COVID-19 found 56 patients had a body mass index (BMI) of 25 to 30, which is classified as overweight.10 Fifty-eight had a BMI of 30 to 40, which indicates obesity, and 13 had a BMI of 40 or higher, which is severely obese. In the study, 71.7% of the critical patients were overweight, obese or severely obese.11
Ultraprocessed Food Impairs the Microbiome
Two studies published by The BMJ in 2019 cast ultraprocessed food as a threat to global public health. In a linked editorial, Australian researchers add that the negative effects of UPFs on the gut microbiome must be explored.12
Science has increasingly revealed the huge effect of diet on the human microbiome and its ability to ward off disease. The more diverse with healthy microorganisms a microbiome is, the better it supports the immune system, according to Tim Spector, professor of genetic epidemiology at King's College in London — especially as COVID-19 has spread all over the world. Writing in The Conversation, Spector says:13
"As well as mounting a response to infectious pathogens like coronavirus, a healthy gut microbiome also helps to prevent potentially dangerous immune over-reactions that damage the lungs and other vital organs. These excessive immune responses can cause respiratory failure and death …
The fine details of the interactions between the gut microbiome and the immune system are not fully understood. But there seems to be a link between the makeup of the microbiome and inflammation — one of the hallmarks of the immune response. Gut bacteria produce many beneficial chemicals."
Fermented foods and probiotics are the best route to optimal microbiome health, if they are traditionally made and unpasteurized. Healthy fermented choices include lassi (an Indian yogurt drink), fermented, grass fed organic milk (kefir), fermented soy or natto and different types of pickled fermentations of cabbage, turnips, eggplant, cucumbers, onions, squash and carrots.
Unless antibiotics are absolutely necessary, they should be avoided and, if avoidance is not possible, counteracted with fermented food and probiotics. Be aware that conventionally-raised meats are also a source of antibiotics because animals are routinely fed the medications. Genetically engineered grains and chlorinated and/or fluoridated water can also destroy gut flora.
UPFs Have Put Millions at Risk for COVID-19
Ultraprocessed food is designed to be sensually appealing, hyperpalatable and habit-forming, thanks to additives, crafty packaging and marketing and "convenience." Yet UPFs fill you up without the vitamins, minerals, live enzymes, micronutrients, healthy fats and high-quality protein your body needs. UPFs increase how fast people eat and delay how "full" they feel, causing obesity and metabolic dysfunction.
Dr. Aseem Malhotra is an honorary consultant cardiologist at Lister Hospital in Stevenage, England.14 According to an article he wrote in European Scientist, UPFs cause:15
"… chronic metabolic disease which can affect many of 'normal' weight. Furthermore, sarcopenic obesity may misclassify many elderly patients to having a normal BMI on hospital admission with COVID-19 … There’s no such thing as a healthy weight, only a healthy person.
A recent commentary In Nature states that 'patients with type 2 diabetes and metabolic syndrome might have to up 10 times greater risk of death when they contract COVID-19' and has called for mandatory glucose and metabolic control of type 2 diabetes patients to improve outcomes."
Kristin Lawless, author of the book, "Formerly Known As Food: How the Industrial Food System Is Changing Our Minds, Bodies, and Culture," also sees correlations between metabolic dysfunction and succumbing to COVID-19:16
"These underlying conditions correlate with increased morbidity and mortality for those who contract the virus. Preliminary findings show that metabolic dysfunction is causing devastating complications from COVID-19 and, shockingly, only 12 percent of the entire U.S. adult population is considered metabolically healthy.
Metabolic dysfunction has one primary source: our highly processed, sugar- laden, nutrient-poor food supply."
While the millions who suffer from metabolic syndrome from UPFs are not seen as urgent like COVID-19 is, the problems are one and the same, according to Malhotra. Governments, in addition to telling people to stay home to save lives during the COVID-19 pandemic, should address diet, he asserts. He writes:17
"[A]n equally strong if not more significant population health message should now be to 'eat real food, protect the NHS and save lives.'
Such implementation backed by policy changes may not just save hundreds and potentially thousands of lives around the world in the coming months but given the high likelihood of another international viral pandemic in the next decade a healthier population … will be much better equipped to handle what would then be a smaller mortality peak on the next occasion."
UPFs Are Especially Harmful to Poor Communities
People living in poverty, whether in developing or advanced countries, are especially vulnerable to health problems from ultraprocessed foods and COVID-19. According to Malhotra:18
"[T]he disproportionate numbers of those from black and ethnic minority backgrounds succumbing to the virus may in part be explained by a significantly increased risk of chronic metabolic disease in these groups."
Even before the COVID-19 pandemic, food giants have targeted those with low incomes with aggressive marketing of UPFs. Following initiatives by Brazil to fight the trend, Ecuador, Uruguay and Peru have urged citizens to avoid UPFs in favor of natural foods.19 Food deserts further the dietary exploitation of the poor, according to Lawless:20
"New data show that Black people are dying at higher rates from COVID-19 than other groups. Certainly lack of health care and poor quality of care shape outcomes, and it is well documented that poverty rates among people of color are significantly higher than in white populations.
Perhaps less obvious is the influence of Big Food’s targeted advertising to people of color in neighborhoods with little access to fresh, whole foods. This means many people of color often rely on fast-food and cheap packaged foods for meals that provide more caloric bang for the buck.
Nationwide, Black people have much higher rates of diet-related diseases — Black adults are 60 percent more likely to be diagnosed with diabetes than white adults."
The USDA defines a food desert as a low-income tract where many residents do not have easy access to a supermarket or large grocery store.21 In addition to a lack of food outlets offering healthy food, residents' lack of transportation to get to stores is a big factor. Residents who have to walk with their groceries or take the bus can carry fewer groceries, and transporting perishable items is especially difficult.
According to the USDA, many types of organizations like businesses, local governments and nonprofits are eligible for assistance to address the problems created by food deserts.22 However, like discouraging the consumption of UPFs, such changes take time and certainly will not occur during the COVID-19 pandemic.
Other Environmental Causes of COVID-19
A diet of UPFs puts people at risk for COVID-19 because of the metabolic, immune system and microbiome degradation it causes. But the coronavirus pandemic also has environmental causes and repercussions, says Lawless:23
"All over the world, industrial agriculture has pushed small-scale farmers deeper into forests where these types of pathogens exist. The decimation of forests has also sent those who bring wild animals into city markets deeper into remote forest areas, resulting in human exposure to novel pathogens.
What’s more, animals confined in factory farms are perfect incubators when these pathogens spill over — unsanitary, cramped conditions among animals with near-identical genetics means that viruses spread rapidly and often become more virulent.”
Whether people whose vulnerability to disease has been increased by Big Agriculture or viruses spread from its excesses, most experts agree we need a radical overhaul of the entire food production and distribution system. According to Lawless:24
"First, our industrial food system is decimating our environment. Second, our nutrient-depleted, and chemically saturated processed food supply is changing our bodies from the inside out …
Large-scale mono-crop farms, concentrated animal feeding operations, fertilizers, pesticides, gas-powered machinery, storage facilities, manufacturing plants, and shipping methods are all dependent on and made possible by fossil fuels … A new Harvard analysis shows that exposure to fine particulate matter correlates with COVID-19 deaths.25
Fuel combustion results in dangerous fine particulate matter, which kills 7 million people prematurely each year worldwide."
If ever there were a time to consider our eating habits and the domination of harmful agricultural systems it is during this coronavirus pandemic.
from Articles https://ift.tt/2ScmY99
via IFTTT
Getting Back to Nature Boosts Natural Killer Cells
During the COVID-19 pandemic, many are asking how they can strengthen their immune system to reduce the potential of getting sick, and how they can support their body if they have a viral infection. As Dr. Roger Seheult explains in this video, natural killer cells are part of your immune response.
While there is no known drug or medication that kills a virus, there are nutraceuticals that have an effect on them. Some of the nutraceuticals support your immune system, while others have the ability to reduce your viral load, as discussed by Mark McCarty and James DiNicolantonio.1
Solar ultraviolet-B radiation2 and supplemental vitamin D3 have also been shown to reduce pandemic fatality rates; this makes sense considering how important vitamin D is for controlling infections and lowering your risk for influenza and the common cold.
How Your Body Uses Natural Killer Cells
Natural killer cells are part of a larger group of cells called lymphocytes. These play a key role in your immune response and defense against viral infections. Inside the cytoplasm of natural killer cells are lytic granules,4 such as granulysin, perforin and granusyme A and B.5
Natural killer cells work by recognizing stressed cells and then using cytotoxic abilities to kill the abnormal cell.6 Once recognized, natural killer cells secrete the granules into a synapse delivering the granules to a target cell. These then trigger apoptosis in the infected cell.
Defects in this system are related to fatal diseases,7 such as Griscelli syndrome type 2.8 This rare, inherited condition affects the immune system, leaving individuals prone to recurrent infections.
Natural killer cells control infection by limiting tissue damage and spread and they help control tumor growth by limiting the spread of abnormal cells.9 They also regulate cells engaged with macrophages, T cells and endothelial cells. Additionally, they can mediate the immune response.
As Seheult explains in the video, natural killer cells are part of the innate immune system, which is the first line of defense against pathogens.10 The next step is adaptive immunity, also called acquired immunity. This response is specific to the pathogen that enters your body. When you build up an immunity to a pathogen, it is the function of your adaptive immune response.
A Forest Walk May Boost Your Body’s Ability to Fight Viruses
Scientific evidence shows that walking in a forest, also called forest bathing, can help enhance your natural killer cell activity, including the number of cells and the length of activity. Research has been done in men and women involving field trips to the forest. In this first study,11 researchers engaged 12 healthy men who normally worked at large companies in Tokyo.
The participants were taken on a three-day, two-night trip to three different forests. On the first day, they walked for two hours; on the second day they walked for two hours both in the morning and afternoon; and on the third day they left for home. Blood was drawn in the morning before any intervention and after the first and second days of walking.
The study team analyzed natural killer cell activity and the proportion of lytic granules and natural killer cells. On the last day, 11 out of 12 of the subjects had 50% higher activity compared to their levels before entering the forest. The researchers believed:12
“Taken together, these findings indicate that a forest bathing trip can increase NK activity, and that this effect at least partially mediated by increasing the number of NK cells and by the induction of intracellular anti-cancer proteins.”
Later, the same team performed the same intervention on 13 healthy women.13 Blood and urine samples were also collected seven days and 30 days after the trip was completed. The team also measured concentrations of phytoncides in the forest, which are airborne chemicals emitted by the plants.
The results of this study showed natural killer cell activity remained raised for more than seven days, as did the number of natural killer cells and the “levels of intracellular anticancer proteins.”
The team questioned whether the effects on the natural killer cells was representative of being outdoors, due to exercise or related to the trees. They designed and executed another study14 with two groups of men who visited two different forests or a city for three days and two nights.
The intervention was the same with blood drawn and urine samples collected before the study began, each day and on Days 7 and 30 after the intervention was complete. During this study they also measured the phytoncides in the forest and the city. As you might expect, measurements in the forest were high, but in the city, most levels were so low they couldn’t be measured. The researchers concluded:15
“The present study confirmed that a forest bathing trip enhances the immune response as measured by human NK activity and the numbers of NK cells, as reported previously. In contrast, a trip to places without forests (city tourist visit) had no effect on NK activity or the numbers of NK cells, indicating that forest bathing does indeed enhance human NK activity.
Moreover, we also found that the increased NK activity and numbers of NK cells induced by a forest bathing trip lasted more than 7 days, even 30 days, after the trip. This suggests that if people visit a forest once a month, they may be able to maintain increased NK activity. This may be important in health promotion and preventive medicine.”
Can You Repeat These Results at Home?
Once the researchers had identified phytoncides as the probable reason individuals were experiencing a higher measure of natural killer cell activity, they designed a follow-up study.16 In this they attempted to recreate the boost in natural killer cells using essential oils from trees.
They engaged 12 healthy men who stayed in a city hotel for three nights between 7 p.m. and 8 a.m. In the morning they returned to work in the city. During the night, researchers ran a humidifier with stem oil from the hinoki cypress tree. “Blood samples were taken on the last day and urine samples were analyzed every day during the stay,” they reported.
Phytoncide measurements in the room were also taken. The study team found there was a statistically significant jump in natural killer cell activity after sleeping in the hotel room, despite the fact they returned to work in the city each day. Urine was analyzed for adrenaline and noradrenaline, since the presence of adrenaline reduces the number of natural killer cells.
Although there was a statistically significant difference in the measurement of adrenaline in the urine of those who stayed in the forest,17 the same difference did not occur in all who stayed in a hotel with stem oil diffused in the room.18
When the data were analyzed together, there wasn’t a statistically significant drop in the excretion of adrenaline in the urine. However, when the researchers separated the samples into those where the adrenaline increased and those where it decreased, there was a statistically significant difference in the reduction of adrenaline in the urine.
They concluded that, while there was beneficial activity to short-term exposure, prospective studies in people exposed to phytoncides long-term would be needed to confirm the effect.
You Also Benefit From Green Spaces
If you don't have a local forest, you can still benefit from exposure to green spaces. In one meta-analysis of 143 studies,19 scientists noted statistically significant reductions in blood pressure, heart rates and levels of cortisol secretion measured in saliva. They also identified decreased incidences of diabetes and all-cause and cardiovascular mortality.
The researchers from the University of East Anglia20 analyzed studies looking at postoperative recovery time. In all, there were 290 million participants across all 143 studies from 20 different countries.
When they correlated the amount of time individuals had spent in green areas with 100 health measurements, they also found that women who were pregnant had a reduced risk for preterm birth and a lower risk of delivering a baby who was small for gestational age.
The relationship may be related to a higher level of physical activity that often comes in green spaces. It could also have something to do with social interaction or greater exposure to sunlight. The researchers concluded:21
“Green prescriptions involving greenspace use may have substantial benefits. Our findings should encourage practitioners and policymakers to give due regard to how they can create, maintain, and improve existing accessible greenspaces in deprived areas.”
Develop Habits to Support Your Immune System
Developing healthy habits is important to support your immune system, reduce the potential for viral infections and lower your risk of chronic disease. While there are multiple choices you make each day, the following factors are foundational to creating a strong health plan.
• Gut microbiome — Your gut microbiota is key to your immune system and digestive health. Fermented food and fiber are vital to repopulating your gut with beneficial bacteria and providing the necessary nutrients for them to thrive.
• Exercise — Research evidence underscores the benefits of exercise to your immune health. Seek to raise your heart and breathing rate for 30 minutes each day in addition to moving out of your chair frequently. Your body requires both exercise and movement to stay healthy.
• Sleep — The quality and quantity of your sleep has a regulatory effect on your immune system.22 Developing good sleep habits requires just a little effort. If you struggle with getting to sleep or staying asleep, consider the tips I share in “Top 33 Tips to Optimize Your Sleep Routine.”
• Vitamin D — This is another powerful component to supporting your immune system and the prevention and treatment of viral infections, including COVID-19. To read more about maintaining appropriate levels and how it may help reduce your risk of COVID-19, see “Vitamins C and D Finally Adopted as Coronavirus Treatment.”
from Articles https://ift.tt/2KKRQJL
via IFTTT
Marked Decrease in Hospital Admissions During COVID Pandemic
A curious thing is happening amid the COVID-19 pandemic: As COVID-19 cases and deaths mount, hospital admissions for other acute ailments are markedly dropping.
In an April 6, 2020, New York Times article, Dr. Harlan Krumholz — professor of medicine at Yale and director of the Yale New Haven Hospital Center for Outcomes Research and Evaluation — notes:1
“The hospitals are eerily quiet, except for Covid-19. I have heard this sentiment from fellow doctors across the United States and in many other countries. We are all asking: Where are all the patients with heart attacks and stroke? They are missing from our hospitals.
Yale New Haven Hospital, where I work, has almost 300 people stricken with Covid-19, and the numbers keep rising — and yet we are not yet at capacity because of a marked decline in our usual types of patients.
In more normal times, we never have so many empty beds … What is striking is that many of the emergencies have disappeared.”
Drastic Reduction in Emergency Admissions
In an informal Twitter poll, created by Angioplasty.org, an online community of cardiologists, 45.4% reported a 40% to 60% reduction in hospital admissions related to heart attacks, and 22.4% reported a reduction greater than 60%.2 Other emergencies, including acute appendicitis and gallbladder disease have also dropped, according to unofficial reports from medical professionals.3 What’s more, according to Krumholz:4
“This is not a phenomenon specific to the United States. Investigators from Spain reported a 40 percent reduction in emergency procedures for heart attacks during the last week of March compared with the period just before the pandemic hit.”
We still do not have an explanation for these statistics. Krumholz hypothesizes that patients may be avoiding face-to-face medical care for fear of contracting COVID-19. If this is the case, their condition may significantly worsen, and lives may be unnecessarily lost.
“As we fight coronavirus, we need to combat perceptions that everyone else must stay away from the hospital. The pandemic toll will be much worse if it leads people to avoid care for life-threatening, yet treatable, conditions like heart attacks and strokes,” Krumholz says.
This isn’t the only possibility, however. As Krumholz notes, natural triggers of heart attacks and strokes may simply have been removed by the imposed social distancing, eating at home and having more time for physical activity.
He’s not convinced that this theory is the most likely explanation, though, considering respiratory infections tend to increase the risk of heart attack. The fear and stress of the situation should theoretically also have led to an increase in heart attacks, as depression, anxiety and frustration “are all associated with a doubling or more of heart attack risks.”5
Delaying Necessary Care Could Cost You
The same story is also reported in an April 19, 2020, article6 in The Washington Post, which notes that:
“Five weeks into a nationwide coronavirus lockdown, many doctors believe the pandemic has produced a silent sub-epidemic of people who need care at hospitals but dare not come in.
They include people with inflamed appendixes, infected gall bladders and bowel obstructions, and more ominously, chest pains and stroke symptoms, according to these physicians and early research …
At [the Medical University of South Carolina, trauma medical director Dr. Evert] Eriksson’s general surgery floor, which has 20 beds, housed as few as three people for two to three weeks, he said. Now the census is back over 20.
‘What we’re seeing is late presentation,’ he said. ‘I would say 70 percent of the appendicitis on my service right now are late presentations. What happens when you present late with appendicitis is we can’t operate on you safely.’”
All-Cause Mortality Is Still Uncertain
Whatever the reason for the drastic decreases in hospital admissions for ailments other than COVID-19, time will tell whether the decrease has actually resulted in increased all-cause mortality or not. As reported by The Washington Post:7
“Much of the reporting about missing patients is anecdotal — in medical chat rooms and on doctors’ social media accounts. Doctors say it’s unlikely there has been a decline in most of these conditions, which suggests that at least a few people may be dying at home, although there is no data yet to corroborate that.”
Some do claim all-cause mortality has risen during this pandemic. According to an April 14 report by The New York Times:8
“Three thousand more people died in New York City between March 11 and April 13 than would have been expected during the same time period in an ordinary year, Dr. Oxiris Barbot, the commissioner of the city Health Department, said in an interview.
While these so-called excess deaths were not explicitly linked to the virus, they might not have happened had the outbreak not occurred, in part because it overwhelmed the normal health care system.”
The New York Times’ claim that the deaths occurred as a result of COVID-19 “overwhelming the health care system” seems suspect, however, in light of so many doctors saying their hospitals are nowhere near capacity.
These conflicting reports show just how difficult it is to tease out the truth without proper data collection and distribution. Without accurate and complete data, it’s virtually impossible to draw any definitive conclusions.
Is Mortality Actually Going Down?
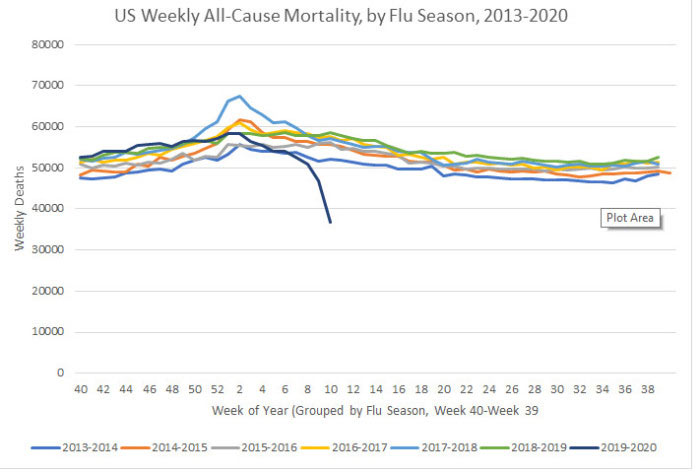
Two interesting graphs created by I. Ratel9 — who freely admits he’s not a statistician or doctor but has degrees in industrial management and automotive technology and whose interest in this is fueled by the fact that he’s immunocompromised — suggest a downturn in both pneumonia deaths and all-cause mortality.
Although final data won’t be released until 2021, I did find in my own research that pneumonia deaths in the current flu season (2019-20) are down compared to 2018-19,10 so I’m including Ratel’s calculations here for anyone interested in diving deeper into his data gathering. Ratel explains the graphs:11
“I’ve been watching CDC’s flu surveillance since last fall when there were rumors floating about of a nasty new flu bug in China … According to the South China Post the first COVID-19 case in Hubei province China was found November 17. Even that article states that patient zero may have been earlier than that …
I contend that it is reasonable to believe that the SARS-CoV-2 virus began circulating around the global population back in November and December, spreading not only across China, but to much of the world.
When considering that possibility, patterns in CDC’s regular ILI (Influenza Like Illness) surveillance data become interesting. I’ve taken their data, and applied my meager Excel skills to chart out some things …
Prior to January we weren’t looking for this virus. We’ve only had useful testing capability for a few weeks now. Given the information we have on disease progression, I assumed that there would be an upward trend in Pneumonia mortality as without looking for and testing for SARS-COV-2, victims should have been classified as deaths due to pneumonia. So, I charted it, with the last 6 years of data published by CDC.
CDC calls week 40 of a year the beginning of the flu season, so all my charts are set to begin in week 40 of one year and end in week 39 of the next, showing years as flu seasons.
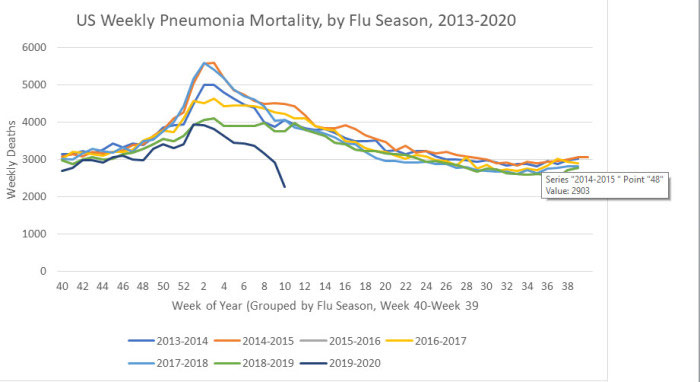
There is the customary increase at week 1, I assume related to holiday festivities and travel. However the 2019-2020 season shows week by week pneumonia mortality to be low compared to the last few years … [and a] sharp decline over the last few weeks.
I next looked at all-cause mortality. Perhaps COVID-19 deaths hadn’t been captured in the pneumonia data … We see here that all-cause mortality ran on the high side of normal until it started to drop at the beginning of 2020, and recently dropped significantly. Again, no indication of this virus killing people beyond seasonal norms,” Ratel writes.
Avoiding Hospitals Might Lower Death Toll
That said, previous research has shown that when conventional medical intervention is reduced, mortality often goes down. For example, back in 2000, all-cause mortality in Israel dropped during a time when Israeli doctors at public hospitals went on strike.12
One of the reasons for this is because medical care itself tends to be a risky business. Research13 published in 2014 found nearly 1 in 5 elderly Medicare patients are injured by their medical care. The most common medical injuries included receiving the wrong medication, having an allergic reaction to medication given, and receiving treatment that led to more complications. As a result of these injuries, they also had a death rate nearly double those who were not injured by their care.
Other research14 published in 2013 concluded 210,000 Americans are killed by preventable hospital errors each year, and when deaths related to diagnostic errors, errors of omission, and failure to follow guidelines were included, the number skyrocketed to an estimated 440,000 preventable hospital deaths each year.
One in 25 patients in the U.S. also contracts some form of infection while hospitalized, and an estimated 205 Americans die from hospital-acquired infections every day. The unfortunate truth is that once you’re hospitalized, you’re immediately at risk for medical errors that might cost you your life. That’s not to say you should never go to the hospital, though.
If you suspect you’re having a heart attack, stroke or appendicitis, for example, you should seek immediate care. Many other ailments that people seek treatment for, however, may simply place them at increased risk for complications.
The difficulty is determining what you might be able to address at home and what’s an actual emergency. If you have access to a holistic physician you trust, calling them for a consultation would be a good idea.
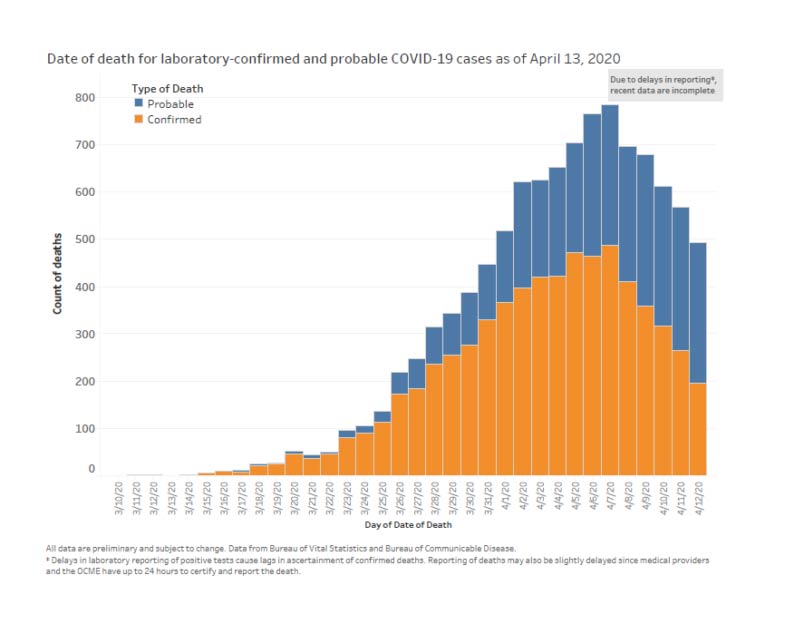
COVID-19 Deaths Jump Due to Reclassification
While other ailments appear to have declined (at least based on hospital admission rates, which may present a false picture of the situation), COVID-19 deaths in the U.S. have undergone a sudden jump mid-April.
While some use this as a sign that the infection is spreading and perhaps more lethal than suspected, the real reason for this sudden jump is simply the reclassification of COVID-19 deaths to include “probable” cases.
While the U.S. Centers for Disease Control and Prevention15 separates confirmed COVID-19 deaths from all-cause mortality, pneumonia deaths, influenza deaths and deaths with both pneumonia and COVID-19, it has issued guidance to states on how to document COVID-19 deaths on death certificates, indicating that COVID-19 should be indicated if “the disease caused or is assumed to have caused or contributed to death.”16
By not requiring COVID-19 deaths to be laboratory confirmed, the death rate can easily become skewed. New York City has officially transitioned its record keeping to include suspected COVID-19 cases,17,18 and as you’d expect, when suspected or “probable” deaths are counted without any proof that SARS-CoV-2 infection was involved at all, the numbers dramatically increase. Ultimately, there is no way to tell what the real impact of the pandemic actually is when using this system.
Looking at the data19 collected for NYC between March 11, 2020, and April 13, 2020, 23.5% of deaths involving residents between the ages of 45 and 64 are in the “probable” category, as are 23.6% of those among 65- to 74-year-olds and 49.9% of those over the age of 75.
As noted by The New York Times20 on April 14, 2020, New York City’s addition of thousands of “probable” cases increased the alleged death rate from COVID-19 by 17% overnight.
Signs of Suicide Epidemic Emerge
Whether all-cause mortality is in fact going up or down, as predicted we are now starting to see a rise in suicides. Suicide statistics reliably follow economic trends, with financial downturns triggering higher rates of depression and despair. According to an updated March 27, 2020, report by The Sacramento Bee:21
“FirstLink, a company that answers both 211 helplines and the National Suicide Prevention Lifeline for North Dakota and parts of Minnesota said this week that call volume in some of its call centers is up 300%.”
According to a spokeswoman for the national Crisis Text Line, text conversations were double that of the normal volume during the week of March 15.22 Google also reports that searches for “panic attack symptoms” have doubled compared to last year.23
The CDC, meanwhile, appears to take things in stride, noting that “Fear and anxiety about a disease can be overwhelming and cause strong emotions in adults and children,” but that “Coping with stress will make you, the people you care about, and your community stronger.”24
While true as a general statement, the current pandemic has delivered a perfect storm of challenges that is sure to bring many to a breaking point. We’re not just talking about fearing a disease. We’re also talking about the very real challenges of keeping a roof over our heads and feeding ourselves and our families when the entire country has been shut down and millions of workers have been laid off.
According to reports by The Federalist25 and Red State,26 suicides exceeded COVID-19 deaths in Tennessee the week of March 20. The Regional Forensic Center in Tennessee was investigating nine suicides as of March 27, eight of which took place in Knox County — one of the few areas in Tennessee where businesses were ordered to close.
The suicides, which occurred within a 48-hour period, account for 10% of the 2019 suicide rate for the region.27 Meanwhile, only six patients died from COVID-19 in the entire state that week. In a statement, Knoxville, Tennessee Mayor Glenn Jacobs said:28
“That number is completely shocking and makes me wonder if what we are doing now is really the best approach. We have to determine how we can respond to COVID-19 in a way that keeps our economy intact, keeps people employed and empowers them with a feeling of hope and optimism — not desperation and despair.”
Similar warning signs are starting to be noted in other states as well, including Oregon. In a March 24 local news report,29 Portland police chief Jami Resch said suicide threats or attempts are 41% higher now than this time last year, and there’s been a 23% increase since the 10 days before a state of emergency was declared in Portland.
Unfortunately, this is likely the beginning of what is most certainly only going to worsen with time, as many financial experts are predicting a depression worse than the Great Depression of the 1930s.30
Suicide Prevention Resources
Clearly, we’re facing an unprecedented challenge, and it’s hard to know exactly what the right thing to do is. There are risks and benefits to every choice. However, I’ve argued since the very beginning that ignoring the human cost of economic collapse is a serious mistake. It’s an equally serious mistake to spread fear unless fear is truly warranted. Mainstream media have a lot to answer for in this regard.
While the future is certainly unsure, I urge you to do what you can to keep yourself on an even keel going forward. Do your best to moderate your fears. And, if you need help, don’t hesitate to reach out to family, friends or any of the available suicide prevention services:
- The National Suicide Prevention Lifeline (U.S.) — Call 1-800-273-TALK (8255)
- Crisis Text Line — Text HOME to 741741 to connect with a crisis counselor
- Lifeline Crisis Chat — Chat online with a specialist who can provide emotional support, crisis intervention and suicide prevention services at www.crisischat.org
from Articles https://ift.tt/2KIrI27
via IFTTT
A state-by-state guide to what you can and can’t do with the easing coronavirus restrictions
from Health | body+soul https://ift.tt/3cUK6kk
Scientists recreate DNA damage caused by toxins from smoking
from Top Health News -- ScienceDaily https://ift.tt/2Yeg4nv
Open access hardware and 3D printing can help tackle demand for health supplies
from Top Health News -- ScienceDaily https://ift.tt/2SeZ7FW
15 ways to boost your immunity (that you haven’t heard before)
from Health | body+soul https://ift.tt/2xgGAS8
How ‘healthy’ is banana bread, really?
from Nutrition | body+soul https://ift.tt/35lQONS
Need to detox? Here’s an F45-approved 15-minute vegan Buddha bowl recipe
from Nutrition | body+soul https://ift.tt/3f3lZBK
A 6-step chocolate and peanut butter ‘cheesecake’ to cure your iso blues
from Nutrition | body+soul https://ift.tt/3aIYbQl
How mistakes help us recognize things
from Top Health News -- ScienceDaily https://ift.tt/3cX4AJ8
How the heart affects our perception
from Top Health News -- ScienceDaily https://ift.tt/2YgiodB
Researchers' method holds promise for brain study, better tests for viruses
from Top Health News -- ScienceDaily https://ift.tt/3f9MANQ
Light-based deep brain stimulation relieves symptoms of Parkinson's disease
from Top Health News -- ScienceDaily https://ift.tt/2yPGHEH
Early high school start times adversely affect attendance
from Top Health News -- ScienceDaily https://ift.tt/2Ye0NmL
Immune-regulating drug improves gum disease in mice
from Top Health News -- ScienceDaily https://ift.tt/2zHxQpf
Smart contact lenses that diagnose and treat diabetes
from Top Health News -- ScienceDaily https://ift.tt/3bMCvnU
Hugs and kisses: Research connects affection, attachment style and marriage satisfaction
from Top Health News -- ScienceDaily https://ift.tt/3f2dPJQ
Visual-spatial learning disorder is more common than thought, finds study
from Top Health News -- ScienceDaily https://ift.tt/2SemHlS
People with brown fat may burn 15% more calories
from Top Health News -- ScienceDaily https://ift.tt/2y7cReT